Living Donor Kidney Transplant
What is a living donor kidney transplant?
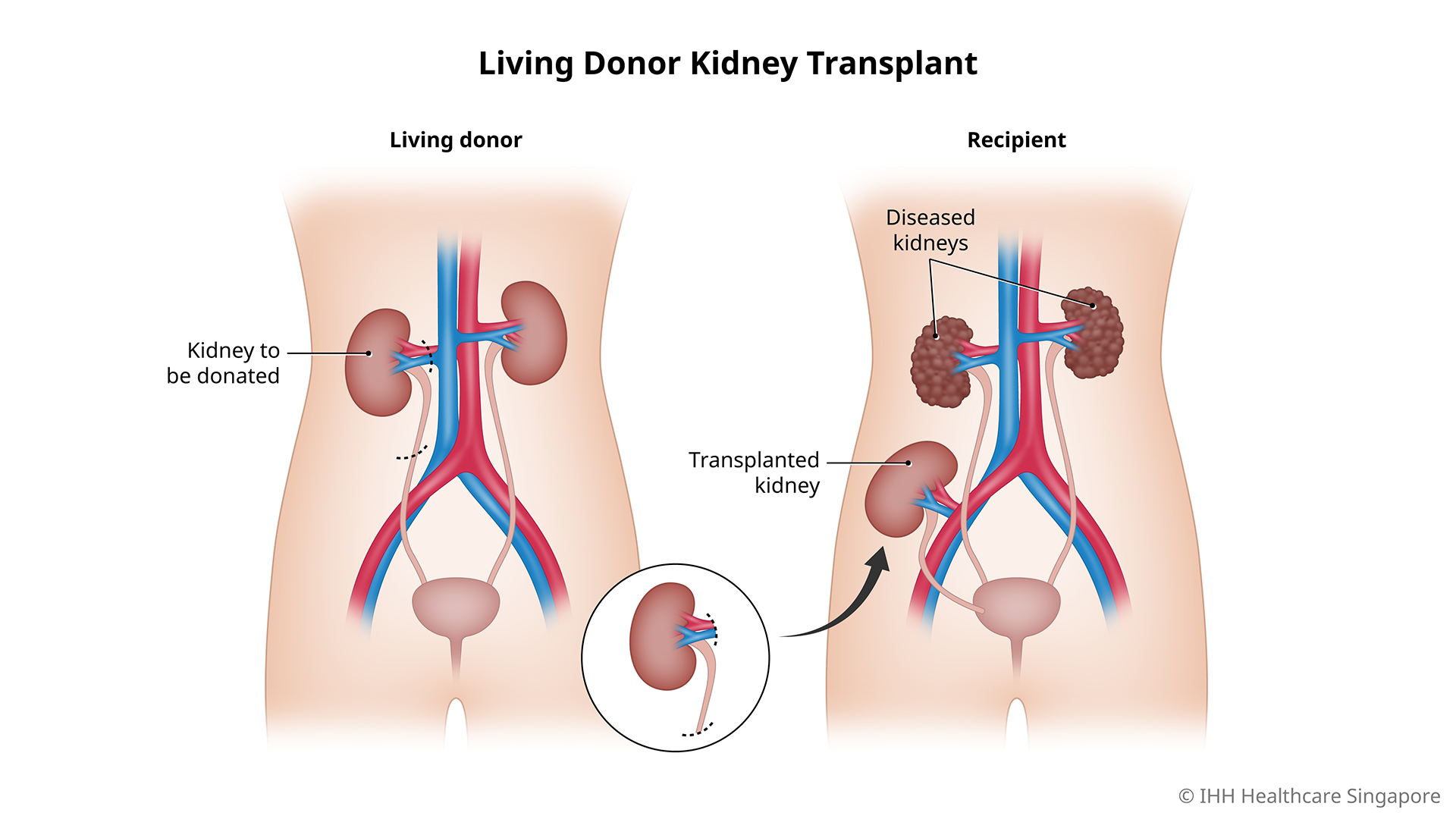
A living donor kidney transplant (LDKT) is an operation where a kidney from a healthy living person (the donor) is removed and placed into someone with end-stage kidney disease (the recipient).
This is usually done without the removal of the recipient's own kidneys.
Why do you need a living donor kidney transplant?
A successful living donor kidney transplant (LDKT) could save your life if you are suffering from end-stage kidney disease. The new kidney can take over the function of the diseased kidneys, and allow your body to self-regulate fluid and electrolyte balance, as well as produce hormones necessary for good bone health and red blood cell production.
The 5 and 10-year survival rates of dialysis vs transplant patients in Singapore are 57.2% vs 93.6%, and 32.7% vs 85.3%, respectively*. This is due to increased cardiovascular complications present in dialysis patients.
(Source: Singapore Renal Registry Annual Report 2019)
Kidney dialysis vs kidney transplant
Compared with dialysis, kidney transplantation offers the following benefits:
- Better survival outcomes, with at least 90% of transplanted patients doing well after surgery
- Better quality of life after receiving a new kidney
- Patients can resume work and normal daily activities
- Patients are free from the pain and complications related to dialysis
- Fewer dietary restrictions
- (For female patients) Higher chances of successfully getting pregnant
Discover the additional benefits of kidney transplantation compared with dialysis, and delve deeper into its viability as a treatment option for end-stage kidney disease.
Deceased donor transplant vs living donor kidney transplant (LDKT)
Compared with a deceased donor transplant, LDKT offers the following advantages:
- Shorter waiting times, with less time spent undergoing dialysis, and even potential avoidance of dialysis in pre-emptive kidney transplantation
- Better graft and patient survival rates
- Ability to schedule your transplant in advance compared to an emergency transplant procedure with a deceased donor kidney
- Blood group incompatible kidney transplantation can be done for some patients
Who should not undergo a living donor kidney transplant?
An LDKT is not recommended if you have any of the following:
- An ongoing infection, which must be treated first
- Severe heart disease
- Cancer that is not in clinical remission
- Active AIDS
What are the risks and complications of a living donor kidney transplant?
For the recipient, an LDKT carries the following potential risks:
- Decreased immunity as a result of the use of immunosuppressants
- Other side effects of immunosuppressants e.g. new-onset diabetes after transplantation, high blood pressure
- Acute rejection, where the immune system recognises the transplanted kidney to be foreign, and begins to ‘attack’ it. This is usually treated with stronger immunosuppressant medications.
- Increased risk of developing cancers, especially certain virus-associated cancers
For the donor, an LDKT carries the following potential risks:
- Risk of death, which affects around 3 – 5 in 1,000 living donors
- Chance of premature kidney failure
- Increased risk of hypertension and/or having protein in the urine later on in life