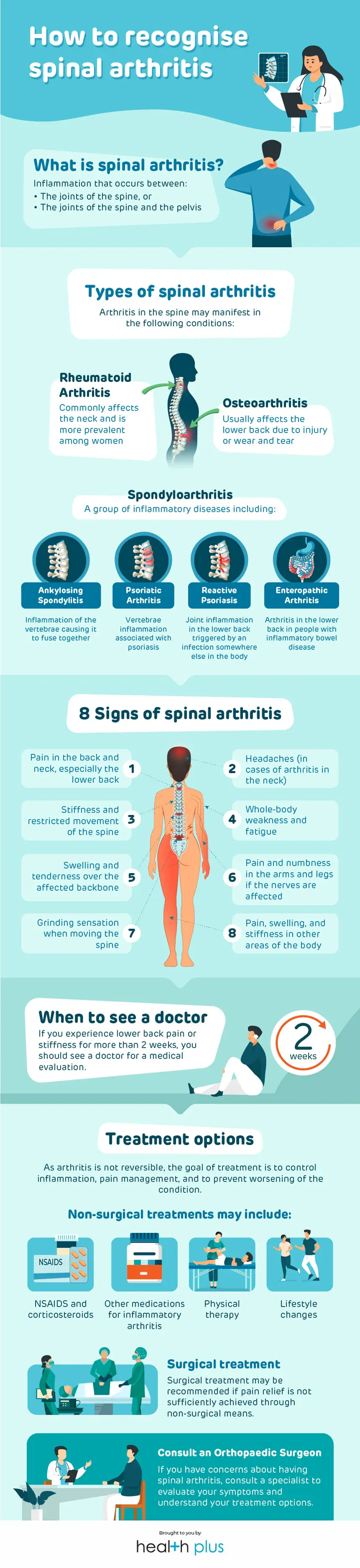
What is spinal arthritis?
Arthritis refers to inflammation of the joints. It is not a single disease, but instead comprises more than 100 types and can affect various parts of the body. Spinal arthritis describes the inflammation that occurs between the joints of the spine or the joints between the spine and the pelvis.
Types of spinal arthritis
Osteoarthritis/ spondylosis
Osteoarthritis is the most common type of spinal arthritis, usually affecting the lower back. It occurs when the cartilage between the joints slowly breaks down due to injury, daily wear and tear, or other joint-related conditions, leading to inflammation and pain.
Rheumatoid arthritis
Rheumatoid arthritis is an autoimmune disorder in which the body’s own immune system attacks the lining of the joints, called the synovium. Commonly seen around the neck, rheumatoid arthritis tends to affect more women than men.
Spondyloarthritis
Spondyloarthritis is a group of inflammatory diseases that affects the joints as well as regions called entheses (where ligaments and tendons attach to the bones). There are several forms of spondyloarthritis, including the following which are more commonly seen in the spine than others:
- Ankylosing spondylitis – Inflammation of the spinal bones (vertebrae) and the joints at the base of the spine that connect to the pelvis. Severe cases result in several vertebrae fusing together, causing a hunched back.
- Psoriatic arthritis – Arthritis that is associated with psoriasis, an autoimmune disorder characterised by itchy and scaly rash. In people with the condition, psoriasis typically precedes arthritis, but the reverse may also occur. Involvement of the spine may result in stiffness due to fusing of the vertebrae.
- Reactive arthritis – Joint inflammation that is triggered by an infection somewhere else in the body (often the genital, urinary, or gastrointestinal system). In the spine, it is usually seen in the lower back and often resolves on its own.
- Enteropathic arthritis – Arthritis that occurs in a small proportion of people with inflammatory bowel disease (IBD). Enteropathic arthritis flare-ups often occur simultaneously with IBD flare-ups, with varying timing and intensity from person to person. In the spine, the lower back area is usually affected.
8 symptoms of spinal arthritis
Symptoms of spinal arthritis differ from person to person. However, they generally include the following:
- Pain in the back and neck, especially the lower back
- Stiffness and restricted movement of the spine
- Swelling and tenderness over the affected backbone
- Grinding sensation when moving the spine
- Pain, swelling, and stiffness in other areas of the body
- Whole-body weakness and fatigue
- Pain and numbness in the arms and legs if the nerves are affected
- Headaches (in cases of arthritis in the neck)
When to see a doctor
If you experience lower back pain or stiffness for more than 2 weeks, you should see a doctor for a medical evaluation.
A diagnosis of spinal arthritis can be broken down to 3 steps. You can expect the following during your consultation with a doctor:
- Medical history taking – You will be asked to describe your symptoms, other medical conditions, current medications, experience with other treatments, family medical history, and general lifestyle habits, eg. exercise, smoking, and alcohol habits.
- Physical examination – Aimed at assessing overall general health, musculoskeletal status, nerve function, reflexes, and evaluation of the problematic joints of the back. Your doctor will be looking at muscle strength, flexibility, and your ability to perform daily living activities such as walking, bending, and reaching.
- Scans and tests – Scans may be ordered to assess the presence or severity of joint damage. This can be visualised with an X-ray. For a more detailed assessment of the spinal canal, spinal cord, nerve roots, discs, and ligaments, a CT scan or magnetic resonance imaging (MRI) may be ordered. Blood tests or testing of the synovial fluid inside a joint may also be used to confirm a spinal arthritis diagnosis.
Treatment options
As arthritis is not reversible, the goal of treatment is to control inflammation, pain management, and to prevent worsening of the condition. Treatment can be divided into non-surgical and surgical approaches, depending on several factors including age, level of pain, and type of arthritis and its severity. It is best that you and your doctor discuss treatment options together and decide on a treatment plan that is most suitable for you.
Non-surgical treatments for spinal arthritis may involve the following:
- Non-steroidal anti-inflammatory drugs and corticosteroids for pain and swelling
- Medications to address specific symptoms or triggers of inflammatory arthritis
- Physical therapy to improve strength of back muscle and mobility of the spine
- Lifestyle changes, eg. losing weight, quitting smoking, and correcting posture, to reduce inflammation or stress on the spine
Surgical treatment may be recommended if pain relief is not sufficiently achieved through non-surgical means. The goals of surgery are to decompress the spinal canal to release nerve roots from bone spurs or other tissues pressed on them and to stabilise the spine through a procedure called spinal fusion.
If you have concerns about spinal arthritis, consult an orthopaedic surgeon for an evaluation of your symptoms and to understand your treatment options.