What is a stent?
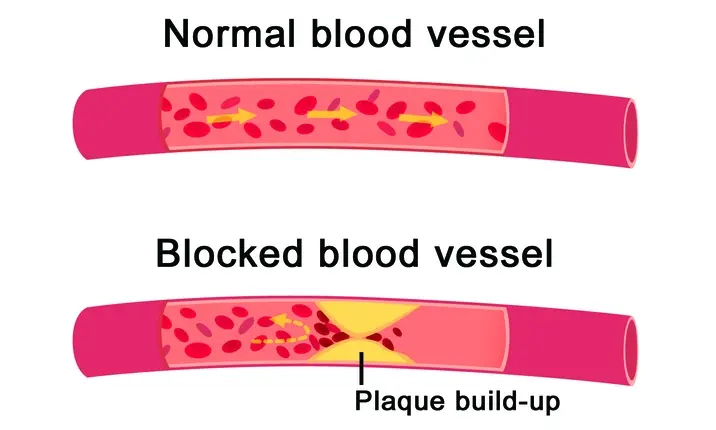
A stent is a small metal or plastic tube used to prop open a blocked passageway. When a build-up of cholesterol blocks a coronary artery, for example, a stent can be used to restore the blood flow and reduce the risk of heart attack.
Stents can also help to prevent aneurysms in the brain as well as open up other passageways in the body, such as bile ducts, lung airways, urinary tubes and leg arteries.
If you think you may need a stent procedure, go for a heart screening or consult a doctor
Why would I need a stent?
Over time, it is common for the arteries, which are vessels that supply blood to and from the heart, to contain a build-up of plaque (a combination of cholesterol and calcium). This plaque can harden, causing blockages and restricting the flow of blood to your major organs. Left untreated, this can lead to conditions such as angina (chest pain) or even a heart attack.
Stents are an ideal treatment choice for patients with heart disease because they are known to have a high success rate. Typically, they are recommended if you have more than 70% blockage in an artery.
Coronary angioplasty and heart stent procedure
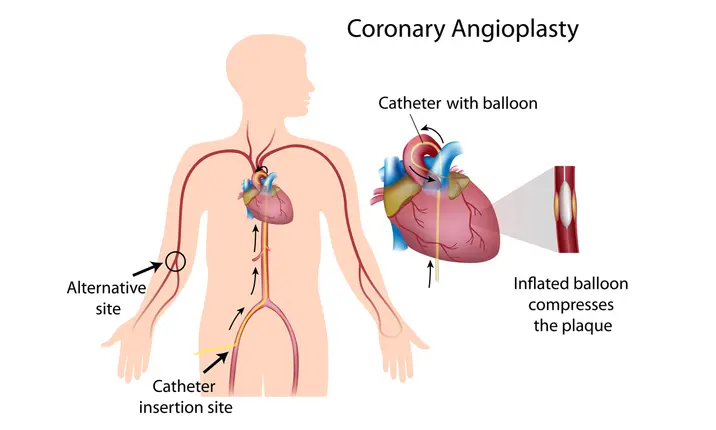
The process of inserting a stent is known as an angioplasty. It's normally a minimally invasive procedure carried out under local anaesthesia.
Firstly, your doctor will perform a cardiac catheterisation, where a thin guide wire followed by a catheter (tube) is inserted into your groin area or arm, through the arteries and towards the heart. A liquid known as 'contrast' is later passed up the catheter to mark on x-rays exactly where the blockages are.
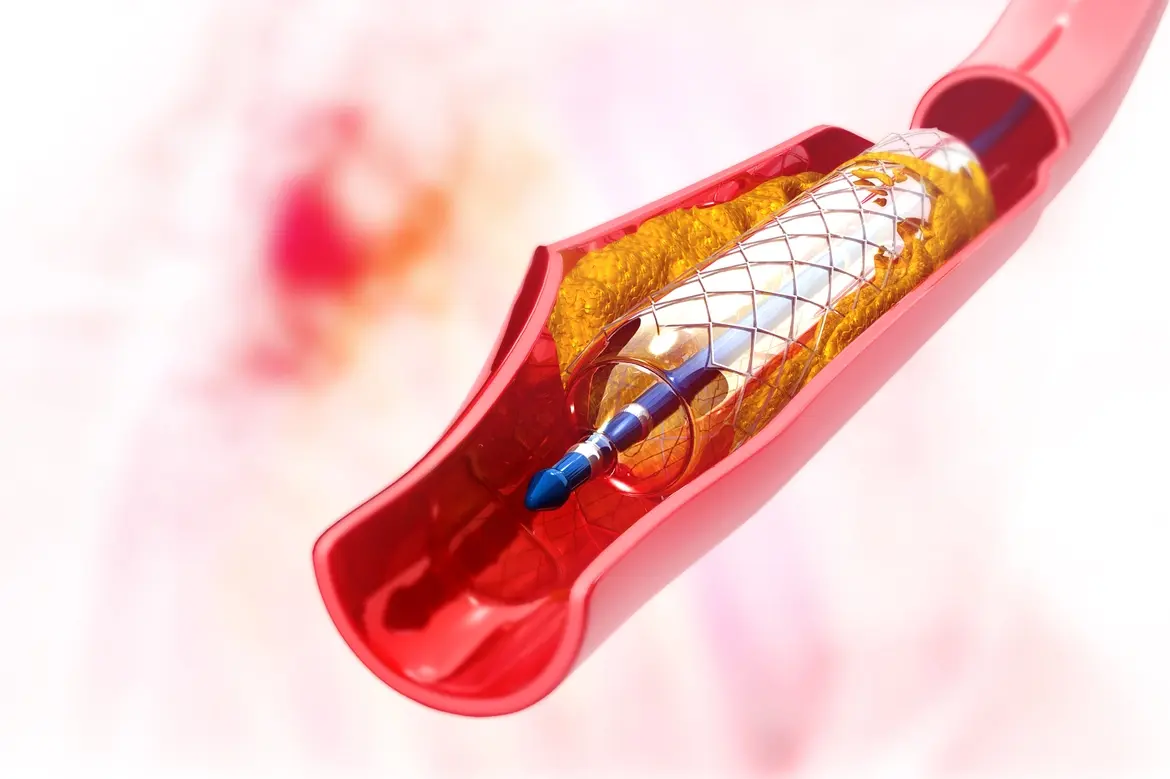
Your doctor will then insert a second catheter, this time with a small, deflated balloon and a collapsed stent wrapped around it. After inflating the balloon to widen your artery, the collapsed stent will expand into place and act as a scaffold for the blocked blood vessel. The contrast will be pumped into your artery again to make sure the blood is flowing properly.
After this procedure, you'll probably need to stay in the hospital overnight so your doctor can monitor your condition.
Types of stents and their uses
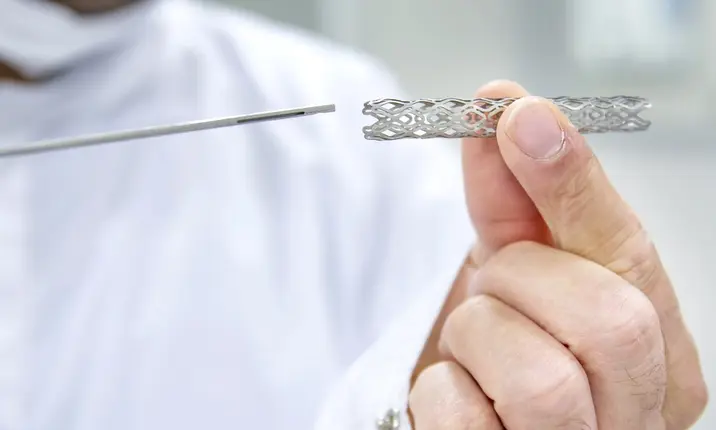
Doctors use several different types of stents, the most common being Bare Metal Stents (BMS), Drug-Eluting Stents (DES) and Bioresorbable Vascular Scaffolds (BVS).
Bare metal stents (BMS)
BMS are the most basic type of stents, containing a stainless steel or chromium-cobalt structure with no added coating. Their main purpose is to prop the artery open and cannot be removed after insertion.
Drug-eluting stents (DES)
DES are made of metals similar to BMS. However, they are additionally coated with drugs that are gradually released into the system to reduce the risk of scar tissue growing in the artery, which could cause another blockage. This added benefit is the reason why they are far more commonly used than BMS.
Bioresorbable vascular scaffolds (BVS)
BVS are fairly new, and unlike BMS and DES, are not designed to be permanent. They are made of a bioabsorbable material such as magnesium or a non-metal polymer, and are also coated with drugs to prevent the artery from re-narrowing. The structure is designed to dissolve in the bloodstream after approximately 2 years, leaving behind no trace of the stent, but ensuring the artery has been sufficiently stretched to prevent blockages from reoccurring.
Other, less common (and more expensive) stent options include:
- Bio-engineered stents: Stents coated with antibodies instead of drugs, which helps to promote the natural healing of the artery
- Dual-therapy stents: The latest generation of stents, combining the benefits of DES, BVS and bio-engineered stents – designed to dissolve, and coated with drugs and healing antibodies
Do stents increase the risk of heart attacks?
A stent can cause blood clotting, which may increase the risk of heart attack. About 1 to 2% of people who have stented arteries have been reported to develop a blood clot at the site of stent.
To prevent blood clotting, doctors will usually prescribe some medications.
What should you do after stent placement?
There are several things that you can do after your stent placement to help ensure good recovery and prevent complications. These include:
- Adhering to the medications that your doctor prescribes. These include blood-thinning medications, such as aspirin and clopidogrel to prevent blood clot formations.
- Continuing with healthy lifestyle habits, including quitting smoking, maintaining a healthy weight, exercising regularly, eating healthy, and keeping other conditions, such as diabetes and high blood pressure under control.
Which is the best type of stent for your clogged coronary artery?
All stents have their advantages and disadvantages. One advantage of BMS, for example, is that you won't need to undergo dual antiplatelet therapy (a combination of blood-thinning medications) for more than a month. However, you will need to keep taking aspirin for the rest of your life, and even then, there's a chance your BMS will fail. In fact, about a quarter of arteries with a BMS stent will close up again within 6 months.
DES stents were specifically designed to counter this issue, and reduce the risk of an artery re-narrowing to less than 10%. If you have a bigger blockage or an additional risk factor like diabetes, you will particularly benefit from this. However, the internal healing process will take longer than with BMS, so you'll need to undergo dual antiplatelet therapy for at least a year after the procedure to reduce the risk of blood clotting.
It might seem like a BVS is the obvious choice – after all, they are well-designed to encourage healing and revert the artery to its natural state – but as the technology is so new, there is a lot more research to be done on its effectiveness. Your doctor also won't recommend them if your arteries have hardened significantly.
"I usually spend a good deal of time discussing the pros and cons of each stent with the patient and family," says Dr Nair. "As BVS are relatively new, they only have over 8 years of data with variable results, and DES have over 10 years of data. BMS have over 20 years of data as they have been used since the 1980s."
"As a general rule, we consider using BVS if the blockage can be treated using conventional stenting. However, since it is a relatively new device, the current use of this stent is confined to simple, less complex blockages. This will continue until more data is available in the coming years and until we gain more experience with this technology."
Learn more about angioplasty, stents and heart health
Some hospitals offer access to high-quality stents and implantation techniques, such as Intra-Vascular Ultrasound (IVUS) and Optical Coherence Tomography (OCT), which can help to ensure you are given the correct stent size and that your doctor can implant the stent successfully. This, in turn, helps to minimise the chances of stent failure later down the line.
If you're concerned about your heart health, remember that going for regular heart screening can help to identify hidden heart risks.
To find out more about angioplasty and stents, or to find the optimal treatment for your heart condition, speak to a specialist.