Breast cancer survival rates are going up, and this is partly thanks to a host of pioneering new treatment options.
Established techniques such as chemotherapy and radiotherapy target both cancerous and healthy cells, leading to a host of serious side effects that impact on quality of life. Whilst they, along with traditional mastectomies, remain an important part of the treatment plan for many breast cancer sufferers, there is a trend emerging among surgeons to employ less radical techniques tailored to the individual patient.
Dr Esther Chuwa, breast cancer surgeon at Gleneagles Hospital, explains what some of these treatments involve.
Removal of breast lumps
Checking your breasts regularly for lumps or unusual tissue texture is important. If you discover a lump in your breast, visit your doctor as soon as possible to get it checked. If your doctor decides to remove the lump for testing, there are a few ways this can be done.
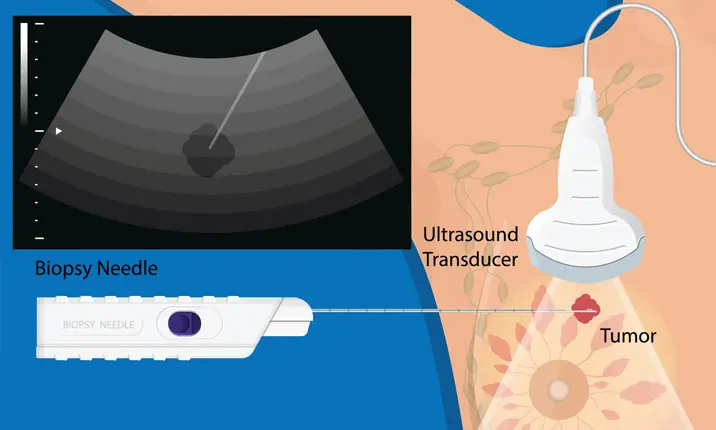
Needle biopsy
A biopsy is the removal of part of an abnormality, such as a lump in your breast, for testing to confirm a diagnosis. These are frequently performed to confirm or rule out cancer.
Dr Chuwa explains, "In the past, an abnormality would have required open surgery to arrive at a diagnosis. Advancements have allowed the use of fine core biopsy needles to extract portions of the abnormality for a full analysis."
This focused technique also means that abnormalities that are too small to be felt, that have been discovered through imaging tests such as mammograms, ultrasounds or MRIs, can also be targeted accurately. Usually performed under local anaesthesia, a needle biopsy only takes 10 – 15 minutes with minimal discomfort.
Vacuum-assisted needle biopsy
This technique introduces a vacuum that draws the tissue into an opening at the needle tip. An automated cutting mechanism cuts the tissue repeatedly in several directions, so that multiple samples can be taken from a single entry.
"This highly efficient technique allows the entire abnormality to be removed under real-time image guidance," Dr Chuwa explains. "By removing the entire abnormality, diagnostic accuracy approaches 100%, removing the need for another surgical procedure."
This procedure is usually indicated with tumours that are probably benign, such as fibroadenomas. More suspicious growths are usually sampled by a core needle biopsy before a planned open surgical treatment, unless doctors can't get enough tissue to confirm a diagnosis. The vacuum assisted needle biopsy takes between 10 – 20 minutes depending on the size of the lesion, with minimal discomfort and scarring.
Minimally invasive cancer treatments
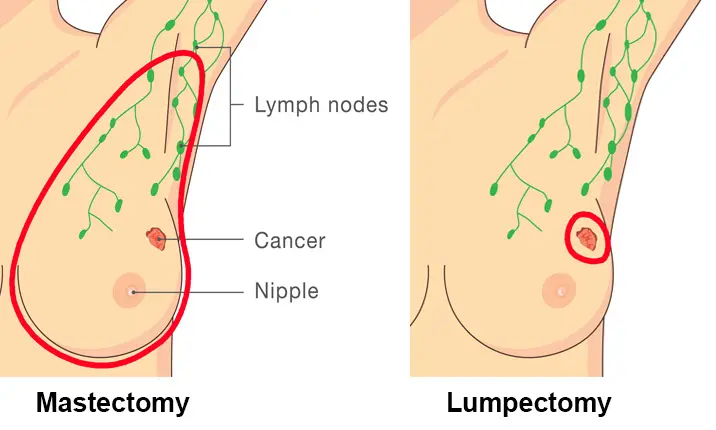
In the early 20th century, radical removal of the breast and all the underarm lymph nodes was the standard treatment for breast cancer. This is no longer the case. If you are diagnosed with breast cancer, there are a number of ways your doctor might choose to treat you. These treatments include:
Cryoablation
Cryoablation is a deep freezing technique that has been used for many years to treat benign breast tumours, as well as cancers of the liver and kidney. More recently, there has been an increase in the use of cryoablation to treat breast cancers.
Dr Chuwa says, "Cryoablation does not just stop at killing the cancer cells upon freezing them. The series of freeze-thaw processes that happen during cryoablation cause the cells to burst, releasing cancer DNA into the system and stimulating an immune response. The immune response then acts as a vaccine to guard against the spread and future recurrence of cancer."
Although still considered experimental, a recent trial conducted across 19 cancer centres in the USA surgically removed cancers previously treated with cryoablation. They found that cryoablation killed 92% of cancers and 100% of tumours smaller than 1cm. If further studies confirm the treatment works effectively and safely, its use may continue to increase to treat carefully selected breast cancer patients. One of the reasons this method is so attractive is that it can be performed in less than 30 minutes at an outpatient setting, under local anaesthesia.
Oncoplastic lumpectomy
Surgical treatment for breast cancer always aims for complete removal of the cancer and minimising the risk of recurrence. Breast conserving surgery (BCS), or lumpectomy, removes the cancer and spares the rest of the breast. Although a full mastectomy is usually recommended if the size of the cancer is too large or if the cancer involves multiple locations within the breast, lumpectomies yield equivalent survival outcomes.
"A successful lumpectomy relies on complete removal of cancer while preserving the natural shape and form of the breast, which may be challenging," says Dr Chuwa. "The concept of an oncoplastic approach to BCS resolves the conflict of clearing the cancer while sparing enough tissue for an acceptable cosmetic result."
Surgeons now prefer to integrate plastic surgical techniques, involving thoughtful scar placement around the nipple or skin folds to minimise scarring, and reconstructing defects using breast tissue flaps or adjacent fat or muscle. Current evidence shows that this approach is safe and results in better cosmetic and patient satisfaction outcomes. Although it takes about 1 hour more than a standard lumpectomy, most patients do not spend longer than a night in the hospital and can resume routine activities the next day.
Skin or nipple sparing mastectomy with immediate breast reconstruction
Mastectomy remains an important treatment option in women with extensive breast cancer or recurring disease, or to reduce risk for carriers of the BRCA mutation gene.
A skin-sparing mastectomy (SSM) involves a standard mastectomy performed through a cut around the nipple but preserves the majority of the native skin envelope. A nipple-sparing mastectomy (NSM) goes a step further by preserving the nipple with no ductal tissue.
Dr Chuwa explains the benefits, "Preservation of the skin pocket, as well as the breast contour, allows surgeons to perform an immediate breast reconstruction with the flap or an implant, and provides an ideal colour and texture match of the reconstructed breast and the opposite breast."
SSM compares to traditional non-skin sparing radical mastectomy both in terms of local recurrence and survival, and offers a much better cosmetic outcome, which is why it is now routinely performed for suitable patients.
Complication rates including flap and implant loss are reported in up to 15% of cases, but vary widely according to surgeon experience and patient risk factors. NSM can be performed as long as the base of the nipple excludes cancer involvement. Rates of post-operative nipple loss range from 2 – 20% but are highly dependent on surgical technique and patient risk factors like smoking.
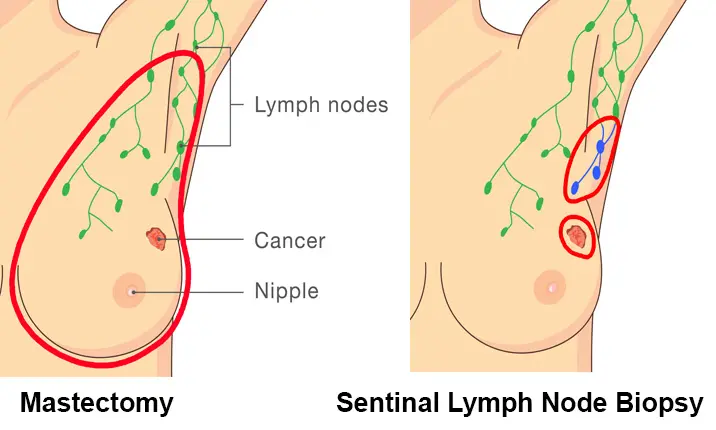
Sentinel lymph node biopsy
The previous trend of removing the breast and all the underarm lymph nodes in breast cancer patients often resulted in cancer recurrence in other parts of the body even when the nodes weren't affected. Research has gradually shed light on the importance of underarm lymph nodes in determining cancer spread.
"Indiscriminate removal of all the nodes is associated with significant side effects including arm swelling or lymphoedema, sensory disturbances and limited arm mobility," explains Dr Chuwa. "Some of these side effects are long-standing and adversely affect the patient's quality of life. If node-negative patients can be accurately identified, they can be spared from unnecessary surgery that does not offer any survival benefit."
A sentinel lymph node (SLN) biopsy aims to identify the sentinel node as the first node to receive lymphatic drainage from the breast cancer. If the SLN is tumour-free, all the other nodes in the nodal basin should also be tumour-free, helping to identify which patients require removal of the lymph nodes. Techniques involve the use of blue dye and radioisotopes, with an identification rate of at least 96%.
Today, SLN biopsies are the standard of care for assessing patients' lymph nodes.
Neoadjuvant chemotherapy and targeted therapies
Breast cancer is regarded as a systemic disease, meaning its effects are on the entire body rather than just one organ or body part, with the potential to spread. It is proven that removal of the cancer alone does not prevent cancer recurrence. Research has revealed that breast cancer cells behave very differently, depending on the genes the cancer expresses, enabling the cells to be categorised into different molecular subtypes.
“Such categorisation allow for treatment to achieve greater precision and lesser toxicity,” Dr Chuwa shares. “By targeting and disrupting specific pathways leading to cancer growth, breakthrough drugs have led to improved outcomes.”
In the past, holistic breast cancer treatment focused mainly on surgery, and uses systemic treatments as follow-up to prevent recurrence. Increasingly, systemic treatments are commenced before surgery (termed 'neoadjuvant') as means to downstage aggressive and advanced disease, and this provides the opportunity for response-guided therapies. Surgeries that follow are usually less radical and yield the evidence of the effectiveness of the systemic treatments on the extent of residual cancer. This in turn helps the physician decide if further treatments would be beneficial.
The future of breast cancer treatment
Research into cancer treatment techniques continues to rapidly advance, offering patients a range of options to improve quality of life and increase survival rates.
"The management of breast cancer continues to evolve towards a paradigm where less is more," says Dr Chuwa. "As doctors gather better understanding of tumour subtypes and the differences in behaviour, we can ultimately tailor more effective treatments for our patients."