Though most colorectal cancers are thought to occur in the elderly, about 5% of cancers occur in those below the age of 44 years, and 18% of colorectal cancer occurs in those below age of 54.
Most people associate passing out blood or constipation with colorectal cancer. However, it is important to know that generally, bleeding or constipation does not necessarily point to cancer, and such symptoms are only exhibited by some cancer patients.
What are the symptoms of colorectal cancer?
Most primary physicians are well aware of the symptoms of colorectal cancer.
The general symptoms include:
- abdominal discomfort
- bloating
- pain
- increased flatulence
Right-sided colon cancer
Patients with right-sided colon cancer display anaemia symptoms due to chronic blood loss:
- Lethargy
- Feeling faint
- Becoming easily breathless due to reduced oxygen in the body
Left-sided colon cancer
Patients with left-sided colon cancer may see changes in bowel habits, such as:
- Constipation
- Abdominal pain
- Stale blood in stools
Rectal cancer
Patients with rectal cancers may experience symptoms such as:
- Diarrhoea, constipation or more frequent bowel movements
- Dark maroon or bright red blood in stool
- A feeling of incomplete emptying of bowels
Early stage cancer
Early stage cancer are commonly without signs. Most polyps (benign growths) and small colorectal cancers do not usually cause symptoms. This is because these relatively smaller lesions do not obstruct stools, especially those on the right side of the colon where stools are more liquid in nature.
Factors that affect colorectal cancer prognosis
There are several factors that affect colorectal cancer prognosis. These include:
Cancer stage
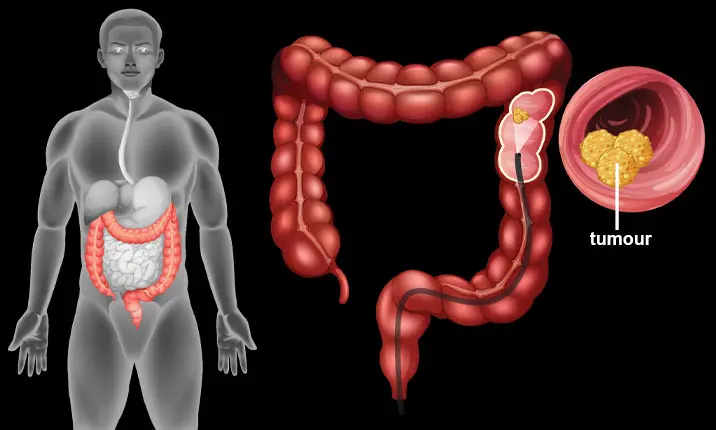
Cancer staging is a system that helps your doctor determine the size of the tumour and if cancer has spread. The number of the stage depends on whether the cancer has spread through the wall of the colon, to lymph nodes and distant organs, with stage 0 representing cancers at their pre-cancerous stage and 4 being the most advanced stage.
Cancers tend to be at an early stage when detected at a screening and there are more people who live at least 5 years after being diagnosed.
Colorectal cancer incidence rises rapidly from the age of 50, and the time taken for a polyp to progress to cancer may be 10 years or more. Hence, screening from the age of 40 allows for the detection of polyps and early cancers.
The recent slight decrease in the incidence of colorectal cancer may be due to increased colonoscopy screening and removal of polyps.
In fact, the best time to prevent colorectal cancer is when there are no symptoms. Early stage colorectal cancer usually presents with no symptoms, and early detection can greatly increase the chances of successful treatment.
Furthermore, it is well accepted that adenocarcinoma, the most common type of colon cancer, develops in the adenoma (a type of non-cancerous growth, or benign polyp). As such, nipping any such benign polyps in the bud is tantamount to treating a future colorectal cancer.
Cancer grade
Cancers are given grades depending on how closely the cancer cells look to normal cells. The more abnormal the cells look, the higher is the cancer grade. Patients with low-grade cancer tend to have better outcomes than those with the high-grade type.
General health
Those who are generally in good health are usually better able to tolerate treatment and its side effects than those who may be less healthy.
Colon blockage
Colon cancer can cause a blockage of the colon or grow through the colon wall and cause a hole in the bowel. Either of these situations can impact your outlook.
Carcinoembryonic antigen
Carcinoembryonic antigen (CEA) is a type of protein present in the blood. The levels of CEA in the blood can increase in those with colon cancer. The presence of CEA at diagnosis may affect how well you respond to treatment.
Detecting colorectal cancer early
Stool occult blood test
Stool occult blood test has been used for mass population screening. The newer tests use antibodies to accurately detect the goblin component in blood.
This compares favourably with the older test which detects haem in the stools – which may require dietary restrictions for up to 3 days prior to testing to ensure that the test is accurate.
These stool tests are able to correctly identify or rule out the disease with 70 – 90% accuracy.
Colonoscopy
For more accurate testing, the colon can be evaluated through a colonoscopy.
The patient has to prepare their bowel by emptying the colon by means of medication the night before.
Though it is commonly held that colonoscopy is invasive and has a risk of puncturing the organ, radiological investigations also carry a (lower) risk of puncturing due to the fact that air has to be used to expand the colon.
Colonoscopy also offers the advantage of sedation, removal of benign growths (polyps) and tissue for biopsies, and it can easily distinguish wounds from the stools sticking to them.
Magnetic resonance imaging (MRI)
An MRI procedure uses magnetic fields to produce detailed images of the body and can be used to measure tumour size. A special dye called a contrast medium is given before the scan, through injection into a vein and / or taken orally as a liquid to create a clearer picture. MRI is the best imaging test to find where the colorectal cancer has grown.
Computed tomography (CT) colonography
CT colonography (also known as virtual colonoscopy) takes pictures of the tumours using x-rays taken from different angles. Images from a CT scan can be used to measure the tumour size. Sometimes a special dye called a contrast medium is given to the patient, through injection into a vein and / or taken orally as a liquid to create a clearer picture. A CT scan can also be used to check whether the cancer has spread to other parts of the body.
Colorectal cancer treatment
Surgery
Surgery still remains the mainstay of treatment of colorectal cancer. With current advancement in medical technology, laparoscopic surgery should be the standard option, with open surgery reserved for those with very large cancers or cancers that have invaded into surrounding areas.
Robotic surgery may have an advantage when dealing with rectal cancers within the confined space of the pelvic cavity.
There are patients who are fretful of having a stoma, an opening to divert faeces or urine to a pouch outside the body. Creation of a temporary stoma is usually reserved for rectal tumours that are near to the anus, whereas a permanent stoma would be required if the anal sphincter is involved by the tumour and had to be removed.
Temporary stomas can be closed as early as 1 month after surgery. For those patients who need a stoma, most stoma appliances can be worn discreetly and it does not leak or smell.
Chemotherapy
Chemotherapy is used after the initial treatment, for stage 3 cancers as well as stage 2 cancers that are at high risk of recurrence.
Radiotherapy
Radiotherapy is used only for rectal cancers, to reduce the chance of recurrence of the cancer.
Survival rate of colorectal cancer patients
Early diagnosis of colorectal cancer saves lives. With improvements in treatment, cancer at earlier stages can often be cured.
Overall, around 64% of people with colorectal cancer live at least 5 years after they receive a diagnosis. However, this 5-year survival rate differs according to several factors, particularly the cancer stage.
Those with localised stage colorectal cancer have a higher 5-year survival rate of 90%. If the cancer has spread to surrounding tissues or organs and/or the regional lymph nodes, the 5-year survival rate is 71%. If the cancer has spread further to distant parts of the body, the 5-year survival rate is 14%.
However, it is important to keep in mind that these rates are an estimate. With better treatment and screening methods, these rates continue to improve.