The statistics tell a chilling story of one of the top cancers in Singapore. Each year, some 1,200 people get diagnosed with colorectal cancer, which is now a leading cause of cancer-related deaths.
Yes, it may be a slow-growing cancer that usually begins as a non-cancerous polyp on the inner lining of the colon, or rectum, but if left undetected, and untreated, colorectal cancer can spread to other parts of the body, causing irreversible harm.
What are the warning signs of colorectal cancer?
Being slow-growing, symptoms do not always show up in the early stages of the disease. In fact, it is often only late in the course of colorectal cancer, that patients begin to notice symptoms. As the cancer advances into its later stages, some patients may begin to notice:
- Changes in bowel habits
- Presence of blood in stools
- Persistent abdominal discomfort such as cramps, gas or pain
- Unexplained weight loss
While conditions such as inflammatory bowel disease, ulcerative colitis, Crohn's disease or even haemorrhoids may result in similar symptoms, these signs should never be taken lightly, especially if individuals fall within the following risk groups.
Who is at risk of developing colorectal cancer?
Colon cancer can affect both men and women. These are some of the usual risk factors:
- Aged 50 or older
- Have a family history of cancer in the colon or rectum
- Have had colon polyps detected
- Have a history of ulcerative colitis or Crohn’s disease
- Smoke excessively
- Have a diet that is high in fat, and low in fruits and vegetables
- Obesity
How does screening help?
Colorectal cancer has a long pre-cancerous stage where small benign polyps may grow in the lining of the colon or rectum. In most instances, they are harmless and will not develop into a cancer. However, there is a chance that some of these polyps may turn cancerous.
This is why detecting and removing them early can play a big role in preventing colorectal cancer. Colorectal cancer in its early stages is highly treatable, so screening is vital for a better outcome.
What are the different screening options?
OBI
Those over the age of 50, or with a higher risk of colon cancer, should take an occult blood immunological (OBI) test once a year. This test detects small amounts of blood in the stool that can't be seen with the naked eye.
In most cases, two fresh stool samples will need to be taken over two days and subsequently sent for testing.
Virtual colonoscopy
In this screening method, a patient first drinks a bowel cleansing solution at home before a CT (computerised tomography) scan on the abdomen and colon is carried out in hospital. Images of the colon are then viewed on a screen by a radiologist. While it’s an option for patients seeking a non-invasive screening method, a virtual colonoscopy will carry a significant radiation risk, and it may miss out the detection of smaller polyps. In addition, if a polyp is seen on virtual colonoscopy, a colonoscopy will be needed for polyp removal.
Colonoscopy
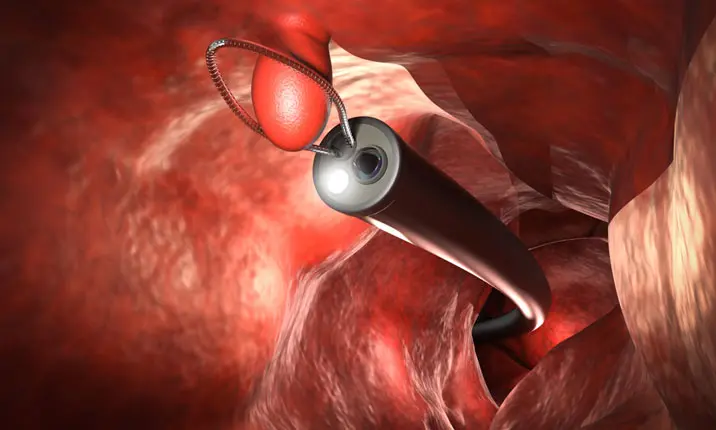
This is the recognised standard for colorectal screening. Undertaken as a day-procedure in hospital, the doctor will examine the lining of your colon by inserting a tube with a camera on the end (colonoscope) into the rectum and through the full length of the large intestine.
Patients will normally be sedated for the procedure, which may last between 20 – 30 minutes. If polyps are present, they will be removed by the doctor during the procedure.
Colonoscopy: Frequently Asked Questions
How to prepare for a colonoscopy?
The patient is required to fast and be asked to take a laxative to clear their bowels prior to the procedure. It is imperative to have an absolutely clean colon before the procedure so that the doctor will not miss any polyps.
What happens after a colonoscopy?
Patients usually recover from the sedation within 30 – 60 minutes following the procedure. There is generally no pain or discomfort during or following the procedure. The doctor will then sit with the patient and explain the findings in detail.
Are there risks with a colonoscopy?
A colonoscopy is generally a very safe procedure. Risk of any bleeding or puncture of the colon if any polyps are removed is miniscule. Bear in mind however, that one may feel a little groggy due to the sedation for a couple of hours after waking up from the sedation.
When should I contact my doctor?
Following a colonoscopy, medical attention should be sought if:
- the bloating continues the next day
- there continues to be blood in the stools
- there is abdominal pain
- there is an onset of a fever over 37.8°C
How often should a colonoscopy be done?
This will be dependent on an individual's age, risk profile as well as personal and family medical history. A doctor will be best placed to advise on screening intervals. In most cases, individuals identified as being 'high-risk' may need to be screened every 2 – 3 years. For those with no history of colorectal cancer, and whose previous colonoscopy was clear, screening intervals can be far longer.
How can colorectal cancer be actively prevented?
While cancer cannot be prevented with surety, the risks of developing the disease can be managed and reduced with good lifestyle habits. These include:
- Eating plenty of fruits, vegetables and whole grains
- Limiting fat in your diet, especially saturated fat from animal sources and plant-based vegetable oils
- Consuming alcohol in moderation, within recommended guidelines
- Quitting smoking
- Exercising regularly
- Maintaining a healthy body weight
Should there be any doubts or questions about your risks of developing colorectal cancer, especially for those aged 50 or older, consider speaking with a gastroenterologist about a colonoscopy and how it can be included into your regular health screening routine.
Should any of the aforementioned symptoms be observed, do not delay making an appointment with a gastroenterologist for an accurate diagnosis and treatment.