Paediatric orthopaedic conditions
Orthopaedic problems in children are common. They can be attributed to a variety of causes that are congenital, developmental or acquired. Some of the origins of acquired orthopaedic conditions in children include infections, nutrition and psychogenic abnormalities.
Clubfoot
What it is. Clubfoot, also known as Congenital Talipes Equinovarus (CTEV), is a birth deformity of the feet that may affect one or both feet. It is relatively common and is in fact, the most common musculoskeletal birth defect.
Symptoms of clubfoot
Clubfoot does not typically cause any discomfort or pain. Signs of the condition include:
- One or both feet pointing downwards or inwards
- Calf muscles in the affected leg(s) may be underdeveloped or tight
- The affected leg may be shorter than the other
Clubfoot causes
Its cause is unknown, but various factors could contribute to this condition, especially genetic factors. It may also be a result of how the foetus is shaped in the womb (intra-uterine moulding).
Clubfoot diagnosis
As clubfoot may be associated with other skeletal conditions, your doctor will perform a clinical examination of your child's spine, hips, hands and feet to accurately diagnose clubfoot and rule out other associated conditions. In 80% of cases, clubfoot is an isolated deformity. In 50% of cases, clubfoot affects both feet.
X-rays and scans are usually not required.
Clubfoot treatment
Treatment varies depending on the type of clubfoot your child has.
- Positional (flexible) clubfoot: As this type of clubfoot involves muscle tightness and/or imbalance (and not the bone), it can resolve itself over time without treatment. Physiotherapy is not required but can be considered as a supplementary measure.
- Structural (less flexible) clubfoot: As this type of clubfoot involves the bones and joints in the foot, leg casting can be very successful as treatment. A groin to toe casting called the Ponsetti casting is used weekly to bring the foot into a normal position. It is usually followed by surgery to release or lengthen the heel cord, following which the child wears special boots connected by a bar to further correct their feet posture.
Non-compliance to wearing these boots as long as deemed necessary may lead to a relapse of clubfoot. Surgical intervention may also be required should casting fail at the start. - Atypical clubfoot: This type of clubfoot is more rigid and serious than the other types, and is characterised by a deep crease across the sole of the foot due to the feet pointing downwards and inwards rigidly.
Casting is unlikely to be successful for this type of clubfoot, and surgery would be required.
Chronic ankle instability
What it is. Ankle sprains are common and comprise approximately 85% of all ankle injuries. They tend to occur in young and sporty individuals, although it can happen to younger children, and people of all ages. Ankle sprains can lead to chronic ankle instability, where the ankle gives way without warning when walking, exercising or doing other activities. Ankle instability can sometimes lead to an early onset of arthritis.
Symptoms of chronic ankle instability
Some symptoms of chronic (persistent) ankle instability include:
- Nagging pain in ankle after standing or walking certain distances despite no recent incident involving the ankle
- Ankle rolling inwards easily
- Ankle feeling unstable
- Persistent discomfort and swelling in the ankle
Chronic ankle instability causes
Chronic ankle instability is typically a result of inversion ankle sprains, where the ankle is sprained as the foot turns inwards. Most of the time, the Anterior Tala-Fibular Ligament (ATFL) is injured, along with the Calcaneofibular Ligament (CFL). These are the ligaments that give us our stability. When these ligaments are unable to properly support us, we may experience ankle sprains frequently.
Chronic ankle instability diagnosis
If the injury is acute, your doctor will physically examine your child's foot and use an x-ray if necessary to check if the ATFL and CPL ligaments display tenderness, or if there are fractures in the foot. This is done when the ankle is not excessively swollen.
If the injury is chronic, a physical examination may not show tenderness over the ATFL and CPL ligaments. However, there may be tenderness over a part of the foot called the Talar Dome. Physical ankle instability tests can be carried out to test if the ligaments in the foot are impaired. In addition to physical examinations, x-ray, Magnetic Resonance Imaging (MRI) and Computerised Tomography (CT) scans can be used to look for cartilage fractures or tears and other injuries that may be present in your child's foot.
Chronic ankle instability treatment
For acute injuries, treatment focuses on restoring stability to the injured ankle, while allowing the pain and swelling to subside. This is done by getting the child to wear an ankle brace, or cast.
For chronic injuries, your doctor will assess if your child's ligaments are impaired and if their ankle instability is worsening. If wearing an ankle brace or cast does not improve your child's condition, surgery may be recommended.
The surgery is minimally invasive, and cuts made to the ankle during the procedure are small. Any injured ligaments are reconstructed and a fibre-optic viewing camera may be used to assess if there are also injuries to the joint. This is a day surgery procedure, and your child will be discharged after the surgery with a walker-boot or cast. Your child can expect to return to normal walking within a month, and sports at 3 months.
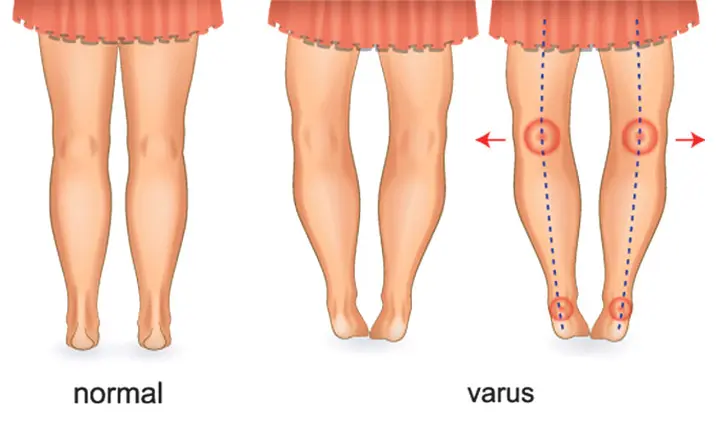
Bow Legs (Genu Varum)
What it is. Abnormal alignment of the lower limbs such as bow legs can be very worrying for parents and is a common problem that parents bring their children to seek medical help for. These conditions tend to be physiological and correct themselves naturally as the child grows.
Physiological bow legs are very common in the child younger than 2 years of age. While bow legs are mostly physiological, there are conditions in which it may not be normal. Most newborns may display bow legs as they begin to stand at 12 – 24 months, or 2 years old. If your child continues to display persistent bow legs after 2 years of age, it is important to seek medical advice to rule out any other causes of bowing.
Symptoms of bow legs
Some symptoms include:
- An obvious gap between the knees when standing straight with feet together
- Worsening deformity over time if left untreated
- There is usually no pain associated with the condition
Diagnosis, causes & treatment of bow legs
There are varying causes of bow legs, and it is usually diagnosed through a physical examination. Blood tests and x-ray scans may also be done where necessary. Some causes of bow legs include:
- Blount's Disease. Blount's disease is an abrupt and progressive deformity of the leg, causing bow-leggedness. This disease is covered in greater detail in this article as the next orthopaedic issue.
- Trauma. Trauma to the leg, especially the thigh bone, can cause abnormal bending of the leg and affect leg growth, leading to deformities. Surgery to correct the deformity involves cutting and realigning bones, or pausing the growth of the longer leg to allow the growth of the shorter leg to catch up.
- Skeletal Dysplasia, or Dwarfism. Your child may have bow legs and a very short stature compared to children his or her age. Surgery can be one form of treatment for bow legs depending on the symptoms and state of the deformity.
- Metabolic Diseases. An example of such diseases is Rickets, a skeletal disorder that is caused by a lack of vitamin D, phosphate or calcium. The disease is associated with short stature and limb deformities such as teeth and skeletal deformities. Bow legs treatment consists of supplementing the missing vitamin or mineral causing the symptoms. Should this be insufficient, corrective surgery may be needed.
Blount's Disease
What it is. Blount's disease is an abrupt and progressive deformity of the leg, causing bow-leggedness. It can affect one or both legs. This occurs when the outer side of the shin bone (tibia) keeps growing, but the inner side of this bone does not. The uneven bone growth causes the shin bone to bend outwards.
Types of Blount's disease
- Infantile Blount's disease: It is generally normal for children under 2 years old to have bowed legs. Infantile Blount's disease may be present if bowing does not improve after age 2 and becomes more severe over time. It affects children aged 2 – 5 years old, usually occurs in both legs and affects the shin bone only. It is more common than adolescent Blount's disease.
- Adolescent Blount's disease. It occurs in children above the age of 10 and affects both thigh bone and shin bone. It tends to occur in one leg only.
Symptoms of Blount's disease
Some symptoms to look out for include:
- Bowing of the leg below the knee
- Knee pain (more common in adolescents)
- Feet of the affected leg pointing inwards instead of straight ahead
Blount's disease causes
The cause of infantile Blount's disease is undetermined. Some people may be genetically predisposed to it as it is hereditary. Infants with Blount's disease also tend to be overweight and early walkers.
Adolescent Blount's disease is strongly associated with obesity and may be caused by rapid weight gain.
Blount's disease diagnosis
Your doctor may use both physical examination and x-ray scans to examine the deformity and its prognosis. For younger children, by examining if the deformity is isolated to the upper part of the shin bone, your doctor will be able to determine if the bowing is due to Blount's disease, or is a normal result of the child's growth.
Blount's disease treatment
It is important to diagnose Blount's disease early as it allows for better treatment and outcome. Children below the age of 3 with less severe bowing may be able to benefit from wearing leg braces. These will have to be worn full-time, especially when walking.
Surgery is likely to be necessary for children whose bowing does not improve despite bracing, are too old for bracing, or whose bowing is more severe. Surgery to correct the deformity involves cutting and realigning bones, or stopping the growth of the longer leg to allow the growth of the shorter leg to catch up. In some cases, bone lengthening is done.
When should you seek a doctor?
If you suspect that your child has any of these orthopaedic conditions, do seek medical advice early for an accurate diagnosis and effective treatment.