Digestive problems refer to any gastrointestinal disorders that occur in the digestive tract, which is also called the gastrointestinal (GI) tract. The first signs of a digestive tract issue commonly include bleeding, bloating, constipation or diarrhoea, and heartburn.
If you're experiencing abdominal pain, nausea or bloating, it could either be a virus that will go away in time, or a sign of a gastrointestinal condition that may require medical attention or a change in lifestyle habits.
You should always consult your doctor to identify the exact cause of your symptoms, but here are a few of the common culprits:
Gastritis
Gastritis is the inflammation of the lining of the stomach. It has many causes, but the most common are infectious agents, especially Helicobacter pylori (H. pylori), aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) like Ponstan, and alcohol.
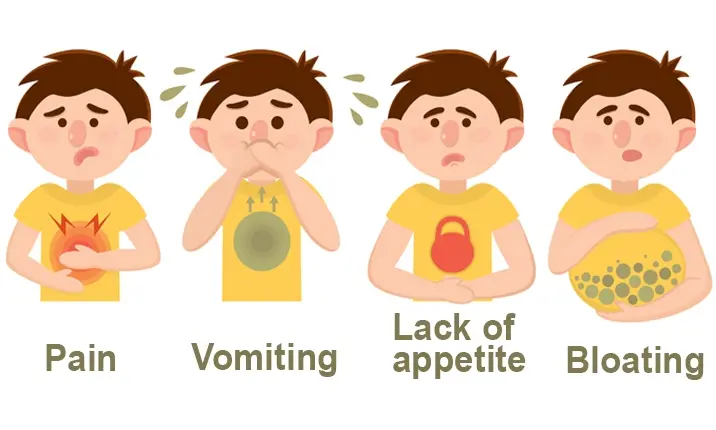
Some common symptoms of gastritis:
- Abdominal pain (intermittent or constant burning, or gripping or gnawing pain)
- Nausea and vomiting
- Loss of appetite
- Bloating, burping and belching
Try to avoid common aggravating foods such as spicy, fatty and fried foods, chilli powder, alcohol and coffee as they may increase the severity of symptoms.
Treatment of gastritis depends on its cause. For gastritis associated with of H. pylori, treatment involves a combination of antibiotics and acid suppressants, while gastritis due to aspirin, NSAIDs and alcohol may require an acid suppressant. Where possible, the consumption of alcohol and the medication responsible for the gastritis should be stopped.
Peptic ulcer
Gastritis is often associated with peptic ulcers. Peptic ulcers are sores that develop in the lining of the stomach, lower oesophagus, or first part of the small intestine. They are usually formed as a result of inflammation caused by H. pylori, aspirin and NSAIDs.
Common symptoms of peptic ulcers
The most common symptoms of a peptic ulcer are upper abdominal discomfort, abdominal pain or bloating. You may also notice loss of weight, loss of appetite, nausea, bloody or dark stools, and vomiting.
With proper treatment, most peptic ulcers heal. However, if left untreated, they can worsen over time and lead to more serious health complications such as a perforated ulcer, a bleeding ulcer (which can cause significant blood loss) or scar tissue that may cause strictures, making it difficult for food to pass through your digestive tract.
Gastro-oesophageal reflux disease
Gastro-oesophageal reflux disease (GERD) is a condition where stomach contents move backwards or reflux from the stomach into the oesophagus. The oesophagus is the tube that connects the throat to the stomach.
Reflux is a normal process that may happen in people who have no bothersome symptoms of acid reflux. In contrast, GERD is diagnosed in patients who have episodes of acid reflux that cause troublesome symptoms.
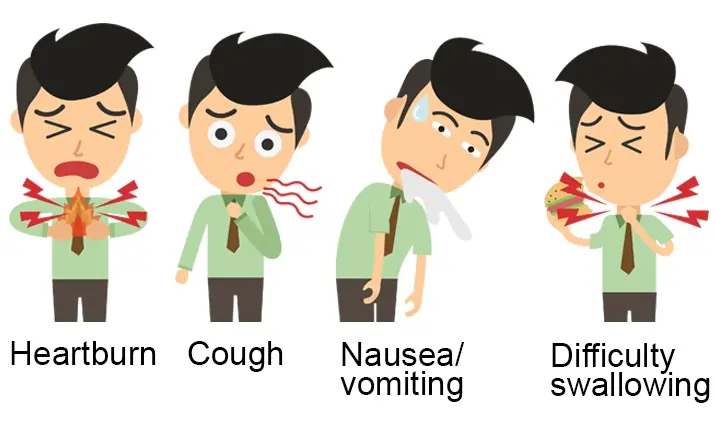
People with GERD may experience symptoms caused by acid irritating and damaging the oesophagus or the back of the throat. These include:
Symptoms of GERD
- Heartburn
- Chest pain
- Regurgitation
- Nausea or vomiting
- Difficulty with or pain when swallowing
- Hoarseness of voice and sore throat
- Cough
Acid reflux occurs more frequently in patients with GERD, compared to those who do not have symptoms of this disease.
It occurs more frequently if the lower oesophageal sphincter (LES), a muscular valve at the lower end of the oesophagus, opens too often or doesn't close tightly enough to keep the stomach contents inside. It happens when you overeat, or when there is too much pressure on your stomach, often due to obesity or pregnancy. Smoking, alcohol and caffeine may also loosen the LES.
Fortunately, symptoms can generally be controlled through lifestyle changes. These include quitting smoking, reducing alcohol and caffeine consumption, eating less fatty foods, and losing weight. In persistent cases, if antacids and anti-reflux medication don’t work, surgery can be a last resort.
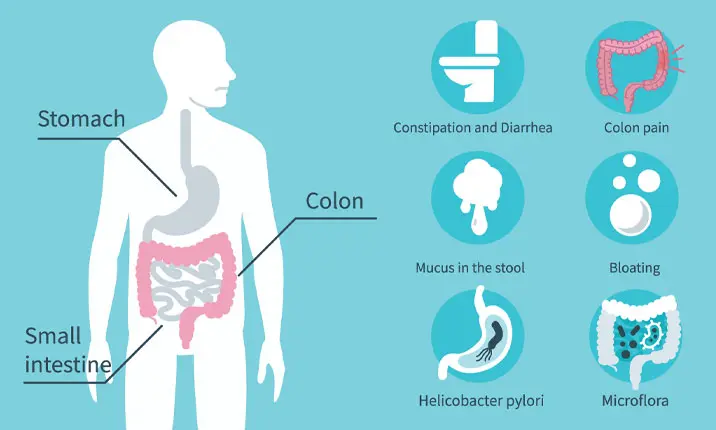
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is part of a group of gastrointestinal disorders known as functional bowel disorders. It is a common problem affecting 10 – 20% of Singapore's population. Patients with IBS have abdominal discomfort or pain that is associated with either diarrhoea or constipation, and the discomfort is usually relieved after bowel movements.
Symptoms of IBS
The symptoms of IBS vary from person to person but are usually present for a long time.
Common symptoms include:
- Pain, cramping, or bloating in the abdomen during bowel movements
- Changes in stool appearance
- Changes in frequency of bowel movements
- Persistent bloating
- Fatigue and difficulty sleeping
Diarrhoea in IBS usually occurs during the day and after meals. Some IBS patients may have constipation instead of diarrhoea and have hard pellet-like stools. Some patients have a combination of both diarrhoea and constipation.
The cause of IBS is unknown. It is often triggered by an episode of gastrointestinal infection or food poisoning. The immune system in the gut is activated during the infection, and produces cells and proteins that increase the sensitivity of the nerves in the gut. The extra sensitive nerves cause the gut to sense normal amounts of gas and movements as bloating and pain.
Stress and anxiety will exacerbate IBS symptoms. However, it is not known if anxiety on its own can cause IBS. Food intolerances are often found in IBS patients but food allergy is not thought to cause IBS.
There is no investigation which will definitively diagnose IBS. Doctors managing IBS patients will often start with a history of the abdominal symptoms and simple blood and stool tests to rule out common disorders. Some doctors may also order more invasive tests, such as colonoscopy and CT scans, if they are thought to be relevant.
Treatment of IBS is aimed at symptom relief and the majority of IBS patients will not require long-term medication. It is usually managed by modifying the person's diet and lifestyle, avoiding foods and other events that trigger symptoms.
Common foods that may aggravate IBS include dairy products, fried foods, indigestible sugars and beans. Some natural foods such as ginger, peppermint and chamomile may help to reduce some IBS symptoms. If lifestyle modification is not sufficient, the doctor may prescribe medication to reduce loose stools, constipation and bloating, or to reduce sensitivity of the intestines.
Read the complete guide to managing IBS.
Chronic diarrhoea
Chronic diarrhoea is defined as frequent loose stools that last for more than 4 weeks.
Causes of chronic diarrhoea
The most common cause of chronic diarrhoea in Singapore is IBS. Another common cause is medicines including antibiotics, painkillers (eg. Ponstan) and diabetic medication (eg. metformin).
Most infections of the intestines cause diarrhoea that lasts for less than 4 weeks. Exceptions include tuberculosis, giardiasis, amoebiasis and tropical sprue, all of which may cause chronic diarrhoea.
In adults, food intolerance may sometimes cause chronic diarrhoea. Lactose intolerance is common in Asians and this can cause diarrhoea and bloating with dairy products. Alcohol and artificial sweeteners may also cause diarrhoea in some patients.
Both non-intestinal and intestinal diseases can cause chronic diarrhoea.
Common non-intestinal diseases that cause diarrhoea include thyroid disease and diabetes.
Thyroid disease
Hyperthyroidism is a condition where the thyroid produces and releases more hormones than is needed. Thyroid hormones are used to regulate metabolism (the process that transforms the food that is consumed into energy), therefore too much of the hormones can result in symptoms related to high metabolism. In some people, an overactive thyroid causes the digestive system to speed up resulting in diarrhoea and more frequent bowel movements.
Diabetes
Some people with diabetes may experience a complication called diabetic enteropathy. In this condition, nerves of the digestive system are damaged, which may lead to diarrhoea. Additionally, diarrhoea may also occur as a side effect of some diabetes medications.
Chronic pancreatitis
Chronic pancreatitis is the persistent inflammation of the pancreas. This can happen due to many causes but the most common one is long-term alcohol abuse. Chronic pancreatitis results in lower levels of pancreatic enzymes and hormones in the body, making it harder for food digestion. One of the symptoms of the condition is diarrhoea.
Coeliac disease
Coeliac disease occurs when the body's immune system attacks its own tissues when gluten is consumed. This causes damage to the intestinal lining, resulting in problems with nutrient absorption (malabsorption). Diarrhoea is the most common symptom of coeliac disease. Malabsorption can also lead to stools containing high levels of fat, causing an unpleasant smell.
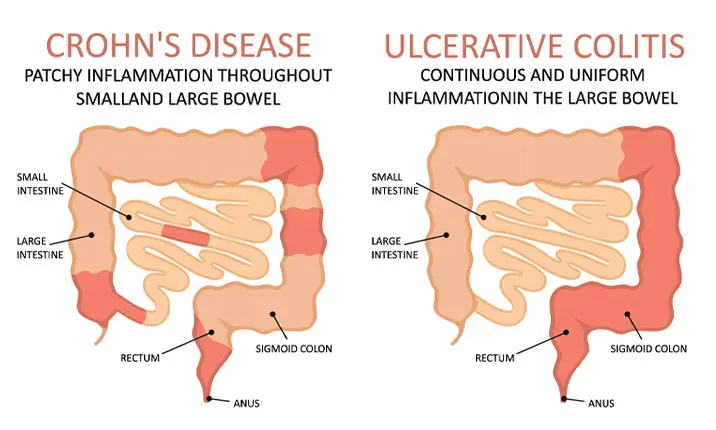
Ulcerative colitis
Ulcerative colitis is a type of chronic inflammatory bowel disease (IBD). In this condition, inflammation and ulcers are present in the lining of the colon and rectum. Bloody diarrhoea is a common symptom of ulcerative colitis. The severity of the symptom depends on the severity of inflammation and ulceration in the colon.
Crohn's disease
Crohn's disease is a type of inflammatory bowel disease causing inflammation and ulcers in any part of the digestive tract. This is a chronic condition where symptoms may develop gradually or suddenly. There may also be periods where no symptoms are experienced. Symptoms of Crohn's disease include diarrhoea, blood in stools and malnutrition.
If you have chronic diarrhoea, your doctor may perform blood tests, stool tests, and, if necessary, a gastroscopy or colonoscopy to diagnose your condition. The preparation process for gastroscopies differs from that of colonoscopies, just as the procedures themselves differ. Ultimately, treatment of your chronic diarrhoea will depend on the cause identified.
Constipation
If you have a decreased stool frequency of less than 3 times per week, hard or small pellet-like stools, or feel the need to strain at stools when passing motion, you may have constipation.
Causes of constipation
There are many causes of constipation. The majority of patients with chronic constipation do not have a disease causing the constipation.
Common causes include:
- Not eating enough fibre, such as fruit, vegetables and cereals
- Not drinking enough fluids
- Being inactive and not exercising
- Often ignoring the urge to go to the toilet
- A change in the diet or daily routine
- A side effect of medications
- Stress, anxiety or depression
Treatment for these patients involve changes in lifestyle, diet and fluid intake, and if necessary, medication.
Non-intestinal diseases associated with constipation include thyroid hormone insufficiency and diabetes. Patients with Parkinson's disease are also more prone to constipation. Some medication including painkillers (eg. morphine) and anti-depressants (eg. amitriptyline) may cause constipation.
If you have constipation, your doctor may evaluate it using blood tests, stool tests, colonoscopy and where appropriate, measurement of anal muscle function.
Treatment for constipation will depend on the cause, and is usually managed by modifying diet and lifestyle, increasing physical activity and fluid intake, and taking natural foods that may help in passing motion (eg. prunes). If lifestyle modification is not sufficient, laxatives may be prescribed.
Inflammatory bowel diseases (Crohn’s disease and ulcerative colitis)
Crohn's disease and ulcerative colitis are collectively known as the inflammatory bowel diseases (IBD).
Patients with ulcerative colitis develop ulcers only in the large intestine. Patients with Crohn's disease develop ulcers in the gut, anywhere between the mouth and the anus. The most common parts of the gut affected by Crohn's disease are the large intestine and the second half of the small intestines.
Symptoms of inflammatory bowel diseases
Symptoms of IBD include abdominal pain, diarrhoea, bloody stools, fever, fatigue, weight loss and malnutrition. In some patients, parts of the body other than the intestines (eg. skin, eyes, joints, or liver) may become inflamed.
Causes of inflammatory bowel diseases
It is not known what causes IBD. It is thought that an environmental factor sets off the gut immune system, which then runs out of control and causes inflammation and ulcers in the intestines of people with the correct genetic predisposition.
There is no cure for IBD as it is a chronic disease. However, it can be controlled with treatment, and patients with controlled disease can still lead normal lives. To diagnose this disease, a series of investigations, including blood tests, stool tests, colonoscopy and CT scans or MRI, will be performed.
If you experience any of the above digestive conditions and are concerned about your gut health, consult a gastroenterologist.