What is an ovarian cyst?
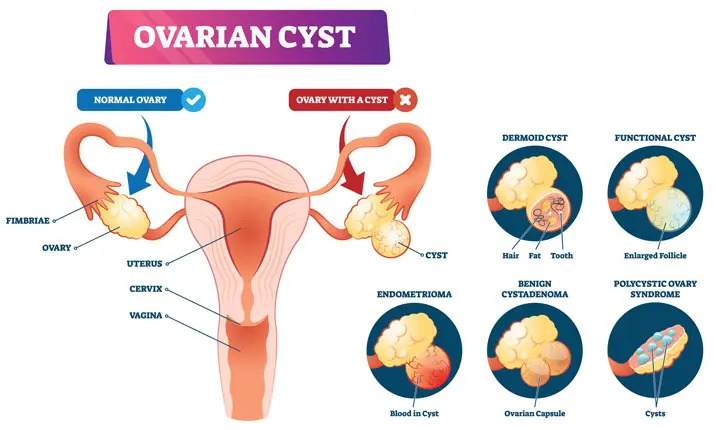
An ovarian cyst is a fluid-filled sac that develops on one or both ovaries. Most ovarian cysts are harmless, non-cancerous, and go away without requiring treatment.
They may develop as a result of underlying health conditions like endometriosis (a painful condition where the cells from the inner lining of the womb grow outside the uterus and in the surrounding areas such as the ovaries, fallopian tubes and ovarian ligaments) or polycystic ovary syndrome (PCOS). There are two main groups of ovarian cysts: benign functional cysts and benign non-functional cysts.
Benign functional cysts
These can be follicle cysts, or corpus luteum cysts.
Follicle cysts may form during a woman's menstrual cycle. During the normal menstrual cycle, a follicle will form and an egg within it will be released once matured. Follicle cyst forms when the follicle doesn't break open to release the egg, causing it to continue growing into a cyst. They often have no symptoms and go away on their own in 1 – 3 months.
Once the follicle ruptures, it becomes corpus luteum. Corpus luteum cyst forms if the sac does not shrink, but instead, fills up with fluid. Most corpus luteum cysts usually will resolve on their own and go away after a few weeks.
Benign non-functional cysts
There are 3 main types of such cysts. Endometriotic cysts, dermoid cysts and cystadenomas.
Endometriomas (endometriotic cysts) are caused by endometriosis. Endometriosis happens when the lining cells of the uterus grow outside of the uterus. When endometriosis is found in the ovary, this may lead to the accumulation of 'menses blood' and this could see endometriotic cysts forming in the ovary.
Dermoid cysts come from cells present in the ovary from birth and do not usually cause symptoms. Fat tissue, bone, teeth, hair and other connective tissues may be found within the dermoid cyst.
Cystadenomas are filled with watery fluid and can sometimes grow very large.
Malignant (cancerous) cysts are rare and they are more commonly found in older patients.
What are the symptoms of ovarian cysts?
Most ovarian cysts are small and don't have any symptoms.
However, if a cyst does cause symptoms, you may feel pressure, bloating, swelling, or pain in the lower abdomen on the side of the cyst.
Painful and ruptured ovarian cysts
The rupturing of a cyst ruptures, it can cause sudden, severe pain. A cyst may also cause twisting of an ovary (torsion), and should it happen, pain will be felt, along with nausea and even vomiting.
How are cysts diagnosed?
Ultrasound
If an ovarian cyst is suspected, an ultrasound scan of pelvis, either trans-abdominal or trans-vaginal may help doctors to confirm the diagnosis.
Radiological imaging
In some cases, further radiological imaging with computerised tomography (CT) or magnetic resonance imaging (MRI) pelvis may be required. In the course of observation, further scans may be advised to monitor the cyst, to determine if it has gone away on its own.
When to see a gynaecologist
If the cyst persists, your doctor may recommend blood tests or refer you to a gynaecologist, especially if there are concerns that the cyst may be linked to cancer. For women who have gone through menopause, the risk of ovarian cancer is slightly higher and may require more regular monitoring.
What kind of treatment is required for ovarian cysts?
Surgical removal of the cysts, known as an ovarian cystectomy, may be advised for women who have gone through menopause or for those who are using birth control pills. It may also be advised if the symptoms are affecting your quality of life or if your ovarian cysts are:
- Increasing in size
- Present in both ovaries
- Persistent and does not go away after several menstrual cycles
- Looks unusual on the ultrasound
- Causes pain
- Potentially cancerous
Left untreated, ovarian cysts can impact fertility, especially if you suffer from endometriosis or PCOS.
For further confirmation, a laparoscopy (a minimally invasive procedure where small incisions are made) or a laparotomy (where larger incisions are made), in the abdomen may be performed to provide your doctor with the best view of the ovaries and determine if you need to undergo an ovarian cystectomy.
What is an ovarian cystectomy?
An ovarian cystectomy is a procedure to remove a non-cancerous cyst. While the ovary is usually left intact, the presence of cancer may require the surgeon to remove one or both ovaries.
Laparoscopic ovarian cystectomy vs. laparotomy
There are two types of ovarian cystectomy procedures, a laparoscopy or a laparotomy, which may be performed under general anaesthesia.
Laparoscopic ovarian cystectomy
Most cysts can be removed using laparoscopy. This is a type of keyhole surgery where small cuts are made in your tummy and gas is blown into the pelvis to allow the surgeon to access your ovaries.
A small, tube-shaped microscope with a light on the end called a laparoscope is then passed into your abdomen. The surgeon then removes the cyst through the small cuts that were made.
After the cyst is removed, the cuts are closed using dissolvable stitches.
With a laparoscopy, you may be discharged and resume normal activity in 24 hours; however, you should also avoid strenuous activity for at least a week or until your doctor gives the all clear.
Laparotomy
A laparotomy may be recommended for cysts that are particularly large or that could be cancerous.
In this procedure, a single, larger cut is made in your tummy. The whole cyst and ovary may be removed and tested in the laboratory to check whether it is cancerous. The incision is closed with stitches or staples.
After a laparotomy, a hospital stay of 2 – 4 days may be required and normal activity may only resume in 4 – 6 weeks.
What are the risks and/or complications of an ovarian cystectomy?
Apart from the risks generally associated with surgery such as bleeding or infection, an ovarian cystectomy may result in scar tissue forming at the surgical site, on the ovaries or fallopian tubes or in the pelvis. Bowel or bladder damage could occur.
It is also possible for cysts to form again on the same or opposite ovary, which is more common in women with hormone imbalances. Full prevention is only possible by removing both ovaries.
How does an ovarian cystectomy affect you sexual health and fertility?
If you have yet to undergo menopause, the doctor will try to preserve your reproductive system by leaving one or both ovaries intact. This means it is possible for you to still produce eggs; if one ovary is removed, you may find it harder to get pregnant. In certain instances, such as suspected or confirmed cancer, it may be necessary for both ovaries to be removed, which means you will no longer produce any eggs. If you have already gone through menopause, both ovaries may be removed.
Who can you see for more information?
Speak to a gynaecologist for more information on ovarian cysts. They will be able to provide an accurate diagnosis and advise on the most suitable treatment options.