What is congestive heart failure?
Congestive heart failure (CHF) occurs when the ventricles (the lower chambers of your heart) become too weak or too stiff to pump blood effectively around the body. This leads to fluid build-up inside your lungs, liver, abdomen and lower body. It is a chronic and progressive condition, which means it comes on slowly and gets worse over time. It can be potentially life threatening.
How can I tell if I have CHF?
CHF is progressive so the symptoms change over time. In the early stages, you may not notice any symptoms at all. The first symptoms that may appear are fatigue, weight gain, swelling in your ankles, feet and legs, and an increased need to urinate, especially at night.
As your condition deteriorates, lung congestion will cause a persistent cough. You may experience an irregular heartbeat and have difficulty breathing and start to wheeze.
When your CHF condition progresses to a very severe stage, your breath will be rapid, your skin may turn blue and you may experience fainting. If you experience any of these latter symptoms, you should get immediate medical care.
What causes CHF?
There are several health conditions that can cause CHF, which is why you should have an annual health check to catch the following heart problems before they develop to this stage.
Coronary artery disease – This is the result of the arteries leading to your heart being narrowed or blocked by cholesterol deposits and other fatty substances.
Hypertension – This is higher than normal blood pressure and can cause heart muscles to become abnormally thickened and stiff, and then weaken over time. It can also lead to coronary artery disease.
Diabetes – Diabetes is also a precursor to heart failure. Diabetes is a leading risk factor for coronary artery disease. Uncontrolled diabetes can also result in a weakening of the heart muscle (also known as cardiomyopathy).
Valve conditions – Your heart valves regulate blood flow through your heart and when they don't open and close properly, it forces your heart to work harder, causing heart damage.
What can I do to slow the progression of CHF?
You should do at least 30 minutes of moderate intensity aerobic activity at least 5 days a week, but avoid exercises that make you feel breathless. Ask your doctor to recommend an exercise routine for you.
Dietary changes are also important to reduce the swelling and slow disease progression. You may be asked to go on a low-salt diet, avoid alcohol and smoking, maintain a healthy weight, control your blood pressure and get enough sleep each night.
What are the surgical treatments available?
If medication and lifestyle changes don't improve your condition, your doctor may recommend a suitable surgical option. Depending on your condition, you may be recommended one of the following:
Implantable cardioverter defibrillator (ICD)
Your doctor may recommend this if you have severe heart failure or a serious heart rhythm abnormality. Your surgeon will implant this "pacemaker-like" device to deliver an electric counter-shock to the heart if a life-threatening abnormal heart rhythm is detected.
Left ventricular assist device (LVAD)
An LVAD is a battery-operated mechanical pump that is surgically implanted to help the heart when it can't pump effectively on its own. This is recommended in "end-stage" heart failure, when the heart is not responding to medication. People who experience persistent breathlessness, recurrent leg swelling or are hospitalised frequently should be considered for this surgery. Your surgeon may also recommend this while you are waiting for a heart transplant.
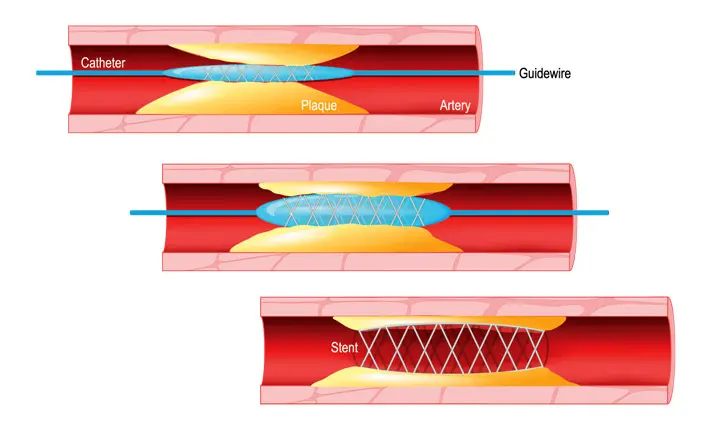
Angioplasty
If your arteries are blocked, your doctor may recommend having an angioplasty, which reopens narrowed/ blocked blood vessels. Your cardiologist will insert a small tube with a tiny deflated balloon on the tip through a small incision in your wrist or groin and push it through towards the diseased artery. Your surgeon then inflates the balloon to open the artery. A stent is usually inserted at the same time to keep the artery open.
This surgical option reroutes the blood supply around a blocked section of the artery. Your surgeon will remove a section of healthy blood vessels from another part of the body, such as one of your legs. These are then surgically attached to the diseased artery so that the blood can flow around the blocked section.
Heart transplantation
Your doctor may discuss a heart transplant as an option if your congestive heart failure is severe and has not responded to medications, dietary and lifestyle changes. If a viable heart is found to be a good match, you will be called in for the operation. During the transplant procedure, you will be connected to a heart-lung machine which will take over the function of these organs so that your surgeon is able to remove the heart and replace it with the donor heart.
The earlier you seek treatment for congestive heart failure, the better your prognosis and quality of life will be. Book a heart screening to check your current heart health and repeat this check-up regularly.