With a vast majority of her population vaccinated against COVID-19, Singapore is gradually transitioning to living with the COVID-19 virus. It's a 'new normal' where COVID-19 is treated as an endemic condition, not unlike the seasonal flu. But this doesn't' come without risks, especially to those with pre-existing medical conditions such as breathing difficulties or chronic lung conditions.
Dr Adrian Chan, respiratory physician and intensivist at Mount Elizabeth Novena Hospital details how the disease may affect patients with underlying respiratory conditions, and what they can do to manage the risks.
How does COVID-19 affect patients with pre-existing respiratory conditions?
Patients with pre-existing chronic respiratory conditions are more likely to become severely ill if they contract COVID-19 infection.
This happens when the virus enters the airways, and lung tissue, through droplet spread and proceeds to infect healthy lung tissue, resulting in inflammation and making it tough to breathe. In patients with chronic lung conditions where there may be pre-existing lung damage, the symptoms of COVID-19 infection can become more pronounced and severe.
Are there specific respiratory conditions that would put patients at greater risk?
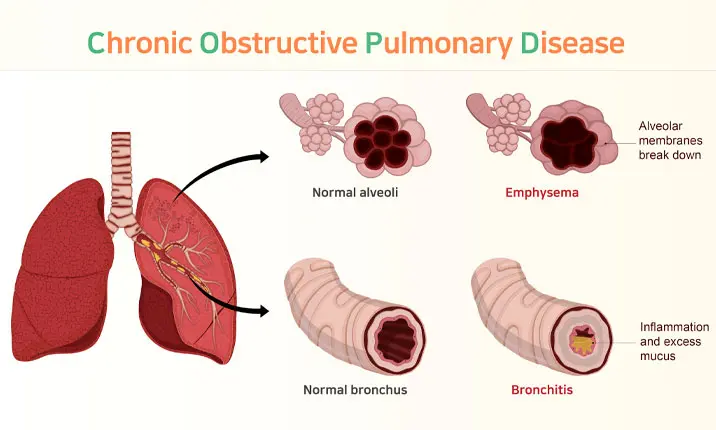
Some conditions that would put patients at greater risk of severe illness include chronic obstructive pulmonary disease (COPD), poorly controlled asthma, and scarred lung tissue from conditions such as interstitial lung disease.
How dangerous will it be for them to contract COVID-19?
For patients with impaired lung function, the additional damage to the lungs caused by COVID-19 may result in severe illness that requires hospitalisation, oxygen support, ICU care and possibly death.
Examples of severe illness include COVID-19 pneumonia, which occurs when the tiny air sacs (called alveoli) in lung tissue become inflamed, resulting in difficulty in the usual exchange of oxygen and carbon dioxide. If COVID-19 affects a significant amount of lung tissue, extensive infection and inflammation can occur and the patient's condition may deteriorate rapidly. Extra oxygen is then required, and sometimes additional intensive care devices/support are required to optimally deliver the necessary oxygen to support the patient's breathing.
Should patients be concerned about getting "Long COVID"?
Yes, "Long COVID" is now recognised as the syndrome whereby symptoms and effects of COVID-19 last for weeks to months beyond the initial illness. In Singapore, about 1 in 10 patients may suffer from this at around 6 months after their infection.
According to the World Health Organisation (WHO), these symptoms may show up in a patient who had initially recovered from an acute COVID-19 episode, or persist on from the initial illness. Such symptoms may also fluctuate or relapse over time.
How does being vaccinated help ease the risk?
Being vaccinated reduces the risk of severe illness during the initial infection, which in turn reduces the risk of getting "Long COVID".
This is because the COVID-19 vaccination allows our bodies to build an immune response to the COVID-19 protein, so that if a patient becomes infected, the patient is able to mount an immune response to the virus, which in turn should reduce the severity of symptoms.
What are some warning signs of a respiratory condition that patients should look out, and seek attention for?
A patient should look out for symptoms such as cough, runny nose, difficulty breathing and/or breathing faster than usual. If a patient is able to obtain pulse oximetry readings, levels below 94% should prompt an evaluation by a doctor.
Particularly for patients who frequently encounter problems breathing, it could point to a chronic respiratory condition if they notice that such respiratory symptoms, such as coughing or breathlessness, are prolonged and progressive and have not improved despite taking simple medications such as cough syrups or lozenges.
How important is it for patients to regularly attend checkups/screenings for their respiratory condition?
Patients with underlying respiratory conditions who remain symptomatic or develop new respiratory symptoms, are strongly encouraged to seek medical attention early.
It is also important to look after one's lung health. Several lifestyle measures that can be adopted include:
- avoid picking up smoking, or quit active smoking
- minimising exposure to environmental pollutants such as dust or fumes
- exercising regularly
- getting vaccinated against flu, or pneumonia
For screening, patients are encouraged to consult a doctor to determine the presence of respiratory symptoms and risk factors, such as active smoking. Several investigations that can be used for screening include lung function testing and radiologic imaging such as a chest X-ray or CT (computed tomography) scan of the lungs.
How can patients manage their conditions, especially in these 'riskier' times?
Currently, hospitals and primary care providers are faced with an increased number of COVID-19 cases and may be stretched. For patients with chronic respiratory conditions who are otherwise well, they may opt to lengthen the interval between their follow ups only if they have sufficient medication and have been adequately educated on how to manage their condition(s) on their own.
What tips can you share for your patients as COVID-19 becomes endemic in Singapore?
Endemic living is only possible if we achieve a high vaccination rate and vulnerable groups (elderly and immunocompromised) remember to receive their booster shots. It is also important for everyone to maintain personal precautions and strictly adhere to public health measures.
Some tips I usually share with my patients include:
- adhering to safe distancing and mask-wearing measures
- avoiding crowded places
- consider regularly self-testing with an ART kit
- encouraging unvaccinated family and friends to get vaccinated