Every one of us has experienced altered bowel habits at some point or another, be it constipation, loose stools or changes in stool frequency or colour. Perhaps you had some 'bad' food. Perhaps you're lactose intolerant and drank too much milk. Perhaps travelling overseas triggered a bout of traveller’s diarrhoea.
For the most part, minor and short-term changes in bowel habits are often harmless. They may be caused by benign reasons such as changes in dietary intake, lack of physical exercise, or taking certain medications. Usually they can be eased by dietary modifications, lifestyle changes and medication if necessary and they resolve reasonably easily.
However, if your bowel problems last longer than 1 or 2 weeks, you may have a chronic condition that requires treatment. If you experience other disturbing symptoms such as severe pain and rectal bleeding, you should immediately seek medical attention to find out if you may have a gastrointestinal disease.
When it comes to gastrointestinal disorders, you would likely have heard of two common terms: Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD).
IBS vs IBD: What is the difference?
What is irritable bowel syndrome (IBS)
Irritable bowel syndrome (IBS) is a very common condition and is estimated to affect around 10 – 20% of the Singapore population.
For most people, IBS is a benign but troublesome condition affecting the large intestine. It is unclear what causes IBS, and only a few suffer severe symptoms. These symptoms may include abdominal pain or cramps, bloating, changes to bowel habits such as constipation, diarrhoea or a mix of both, incomplete or unsatisfactory bowel movements or changes in stool consistency.
What is inflammatory bowel disease (IBD)
Inflammatory bowel disease is an umbrella term for disorders involving chronic inflammation of the gastrointestinal tract, namely ulcerative colitis and Crohn's disease.
These inflammatory conditions mean that the intestinal wall becomes swollen and develops ulcers. Over time, this can lead to serious damage to the digestive system. Symptoms of IBD typically include abdominal pain, diarrhoea, bloody stools, fatigue, and weight loss. Although less common than IBS, IBD has become increasingly prevalent in Asia over the last decade – there are an estimated 2,000 patients in Singapore today.
Types of Inflammatory Bowel Disease
There are 2 main types of inflammatory bowel disease: Ulcerative colitis and Crohn's disease.
Ulcerative colitis
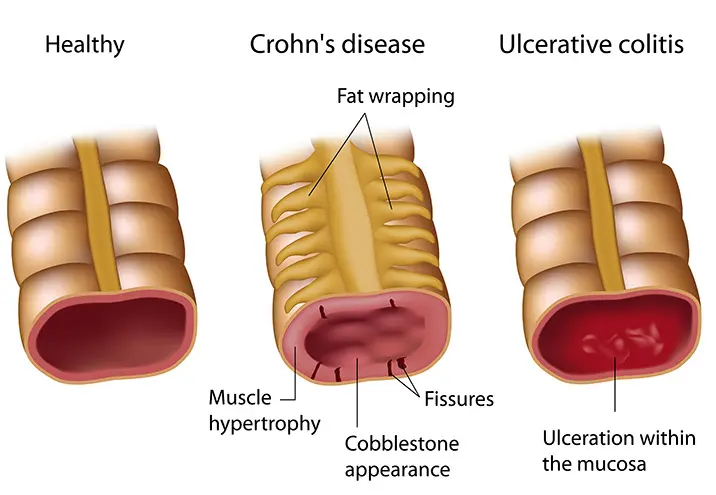
Ulcerative colitis, as its name suggests, occurs only in the colon, also called the large intestine. While the inflammation can range from mild to severe, it always starts in the rectum but can affect the entire colon.
It is marked by continuous inflammation and, if in severe cases, ulceration of the colon, typically at the innermost lining. The more affected the colon is, the worse the symptoms will be.
Crohn's disease
Unlike ulcerative colitis, Crohn's disease can affect any part of the gastrointestinal tract, from the mouth all the way to the anus. Instead of continuous inflammation, inflamed areas appear in between healthy parts of the intestine. Crohn's disease can occur in all layers of the bowel walls, presenting as either shallow crater-like areas or deep lesions, leading to complications such as scarring and stricture of the intestines as well as abnormal connections between loops of intestines, called fistulae.
Ulcerative colitis vs Crohn's disease: What's the difference?
It is important to note that while IBS and IBD share some overlapping symptoms (such as abdominal pain and diarrhoea), they are actually completely different conditions. IBS is a benign syndrome, meaning that while it comes with a constellation of bothersome symptoms, it does not lead to serious health issues or complications, although quality of life may be significantly affected.
IBD, on the other hand, is an inflammatory disease, meaning that it is potentially much more debilitating and can lead to serious complications such as severe bleeding, obstruction or rupture of the intestines. In some cases, it is related to the development of cancers such as of the colon or bile ducts.
| Ulcerative colitis | Crohn's disease |
| Occurs in the colon | Occurs anywhere in the gastrointestinal tract, though most commonly at the tail end of the small intestine |
| Affects only the innermost lining of the colon | Affects all layers of the intestine walls |
| Inflamed area is continuous | Inflamed areas may appear in patches next to healthy parts of the intestine |
| Possible complications: perforated colon, toxic megacolon, severe dehydration, colon cancer | Possible complications: bowel obstruction, fistulae, anal fissures, malnutrition, colon cancer |
Both ulcerative colitis and Crohn's disease can strike at any age, though they are most commonly seen in teenagers and young adults aged 15 – 35.
What are the symptoms of inflammatory bowel disease?
The symptoms of inflammatory bowel disease can vary, depending on the level of inflammation and where it is located.
The signs and symptoms of both ulcerative colitis and Crohn's disease are largely similar, including but not limited to:
- Abdominal pain and cramping
- Bloating or distension
- Blood or mucus in the stools
- Loss of appetite
- Persistent diarrhoea
- Fever and fatigue
- Unintended weight loss
- Inflammation of the skin, eyes or joints
- Delayed growth and sexual maturity in children
These symptoms may come and go or be progressively more severe. IBD patients may experience flare-ups, when the disease is active and the symptoms are very severe, or they may undergo periods with few or no symptoms at all, when the disease is in remission, usually after appropriate treatment.
If you have persistent, bothersome symptoms related to the abdomen and the bowels or associated systemic symptoms such as lethargy, loss of appetite or weight, speak to a gastroenterologist, who will help to identify the cause of your bowel symptoms.
Diagnosing inflammatory bowel disease
To help diagnose inflammatory bowel disease, your doctor will take note of your medical history and symptoms, and recommend some diagnostic tests.
These tests can range from relatively non-invasive procedures (such as a blood and stool tests) to imaging (such as CT scans and MRI) to minimally invasive procedures (such as gastroscopy and colonoscopy).
Making an early diagnosis of IBD is important as any delay can lead to a higher risk of complications. IBD patients also do less well if their condition has been poorly controlled for a long period of time. It is equally important to exclude serious diagnoses such as IBD and make a clear and confident diagnosis of IBS so that this can be managed appropriately to improve quality of life.
Treating inflammatory bowel disease
Treatment of IBD depends on the severity of the disease and its responsiveness to available therapies.
Anti-inflammatory medication
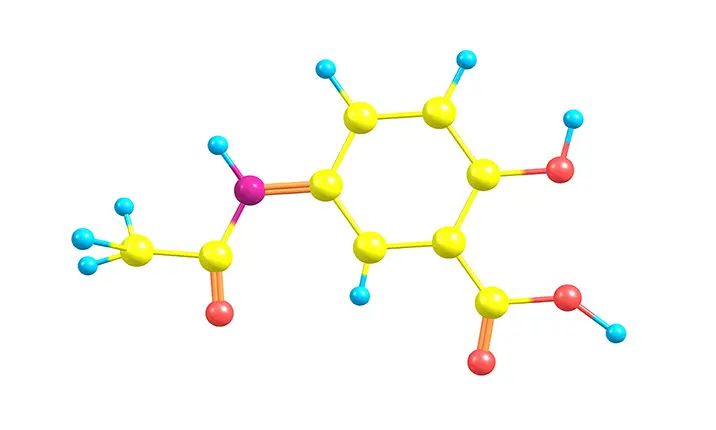
Mild ulcerative colitis may be controlled with anti-inflammatory medication such as Mesalazine.
Immunosuppressive medication
Patients with more severe inflammation may require treatment with immunosuppressives such as corticosteroids (prednisolone or hydrocortisone). Other immunosuppressive drugs such as Azathiaprine or Methotrexate may be substituted to avoid the long-term side effects of corticosteroids.
For some patients, biologics may be recommended – these are powerful molecules injected either intramuscularly, intravenously or subcutaneously. This form of treatment targets specific proteins that cause inflammation and help to actively suppress the immune system.
As with all drugs, there are potential side effects to be aware of. Since treatment is often lifelong, your gastroenterologist would have a serious discussion with you on which medications will help to treat the inflammation, and for how long.
Surgery
In severe cases of IBD, where the disease isn't responding to medication or where the patient’s life is in danger, surgery may be necessary as the last resort. According to estimates, around 25% of patients with ulcerative colitis and up to 75% of patients with Crohn's disease will require one or more surgeries in the course of their lifetime to help treat their IBD.
In general, the earlier IBD is diagnosed and controlled, the less likely patients will require surgery. Consult a gastroenterologist if you’re concerned you may have IBD or any other digestive conditions.