We look at how having a gastroscopy or colonoscopy can help screen for, and even prevent cancer, and how these procedures play a part in the early treatment of these conditions.
Differences between a gastroscopy and a colonoscopy
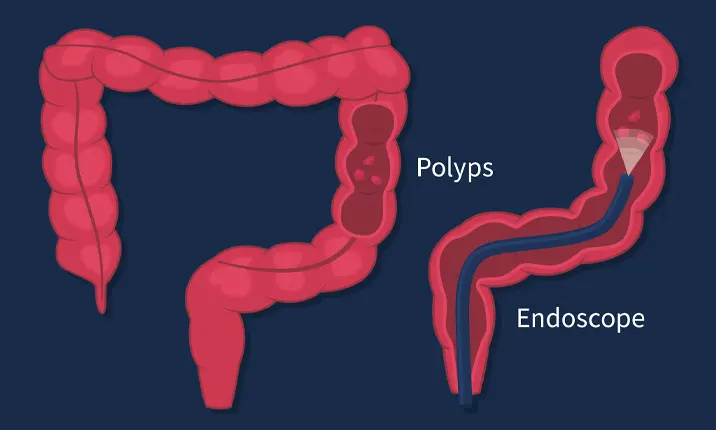
First things first, both gastroscopies and colonoscopies are known as endoscopic procedures. Endoscopy refers to the visual examination of our body cavities using long and thin flexible telescopes that are attached to a video monitor. The procedure is called a gastroscopy when the scope is inserted through the mouth to examine the stomach. When it happens from the anus in the examination of the colon and rectum, it is called a colonoscopy.
Let's look at each procedure in greater detail:
Gastroscopy procedure
Gastroscopy looks at the upper gastrointestinal tract. A gastroscopy usually takes around 10 minutes and is carried out by a doctor who specialises in gastroenterology or gastrointestinal surgery. You are required to fast for 6 hours prior to the procedure. You will be asked to lie on your left side and an intravenous sedative will be given. Upon 'falling asleep' the scope will only be inserted is only inserted through your mouth and passed gently into your oesophagus, stomach and duodenum.
Colonoscopy procedure
Colonoscopy is used to examine the lower gastrointestinal tract. The scope is inserted through the anus and passed up to examine the rectum and entire colon. The procedure lasts around 30 minutes and is done under sedation. Air is used to inflate the bowel so that the examination can be more accurate. You may feel some discomfort from the bloating but there should not be any pain. The day before your colonoscopy, you will be asked to consume a low residue diet and avoid any fruits and vegetables. A bowel preparation laxative will also be given to help clear the bowels for a better view of the large intestine. Depending on the timing of your procedure, the bowel prep may be given the night before or on the morning of your colonoscopy.
Can an endoscopy detect cancer?
Endoscopies are most commonly used in the screening and detection of diseases and conditions, but they may also be used to help carry out certain treatments. These include the control of internal bleeding, biopsies – the removal of tissue samples for further analysis in the lab – and in the removal of polyps – precancerous growths that can lead to cancer.
Your doctor may recommend a gastroscopy or a colonoscopy to screen for stomach or colon cancer. The aim of screening is to detect cancers at an early curable stage even before you have any symptoms.
Colorectal cancer is now the most common cancer in Singapore. The majority of these cancers start as little polyps that take about 5 – 10 years to grow and undergo cancer change. 9 in 10 colorectal cancers can be prevented with regular colonoscopy screening at 5-year intervals, starting from the age of 45.
Detecting stomach problems
Besides cancer screening, gastroscopy and colonoscopy are also frequently done for the accurate diagnosis of digestive or stomach problem symptoms so that precise medical treatment can be given.
Stomach symptoms that require a gastroscopy
Your doctor may recommend a gastroscopy if you show symptoms of stomach problems such as:
- Abdominal pain or discomfort that is persistent
- Difficulty in swallowing or vomiting
- Heartburn or reflux symptoms
- Indigestion and/or bloating after meals
- Passage of black stools (this may be due to internal bleeding in the stomach)
- Loss of appetite and weight
Symptoms of stomach problems that require a colonoscopy
Your doctor may recommend a colonoscopy if you show symptoms of stomach problems such as:
- Abdominal pain or discomfort that is persistent
- Change in bowel habits, such as constipation or diarrhoea
- Passage of mucus or blood in the stool
When should I go for a colonoscopy or gastroscopy?
When symptoms are present: If you display any of the symptoms mentioned above, you should book an appointment with your doctor to obtain an accurate diagnosis.
Preparing for your endoscopy
Gastroscopy and colonoscopy are usually done as day procedures with overnight hospitalisation not required. You will be asked to report an hour before the procedure time.
You will be sedated during the procedure and you will wake up in the recovery ward once the procedure is over. You will be given a light snack and adequate time to fully awake before going home. It is best to have someone accompany you home as you should not drive after having sedation.
Your doctor will review you before your discharge and discuss the scope findings and further treatment plan with you.
If you are concerned about symptoms or would like to book a screening, consult your gastroenterologist to get an accurate diagnosis.