What is gestational diabetes?
Gestational diabetes is a type of diabetes that develops only during pregnancy, commonly between the 24th and 28th week. It is accompanied by unusually high blood sugar levels.
Although the condition will usually resolve after your baby is born, your risk of developing type 2 diabetes later on in life is significantly higher.
Proper management of your blood sugar level is not only essential for your health, but for your baby’s as well.
What are symptoms of gestational diabetes?
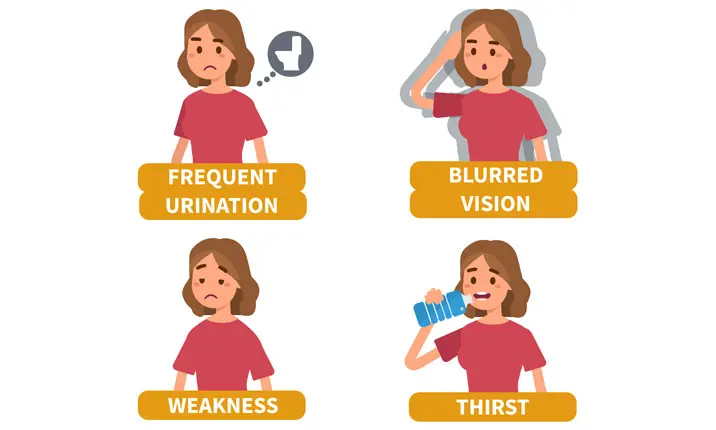
The symptoms of this condition are similar to that of non-pregnancy-related diabetes.
- Blurry vision
- Constantly feeling thirsty
- Feeling tired all the time
- Frequent urination
What causes gestational diabetes during pregnancy?
The exact science behind why some women develop gestational diabetes during pregnancy while others do not is still not fully understood. However, it is important to know how your pregnancy can affect your body’s glucose regulation.
Normally, glucose in the food you eat is absorbed into the bloodstream. Your pancreas responds to this increase in blood sugar level by producing insulin, a hormone that allows your body to use sugar from carbohydrates in the food that you eat or to store the excess glucose in the liver.
While you are pregnant, your body increases the production of other different hormones which can reduce the ability for insulin to carry out its function, causing your blood sugar level to become unregulated, leading to diabetes. An unregulated blood sugar level can have adverse effects on the development and health of your baby. It may also increase the risk of complications such as high blood pressure, premature delivery or an unplanned caesarean during delivery.
Glucose screening test for pregnancy
A glucose screening test measures your body’s response to sugar (glucose). It is used to screen for gestational diabetes, a specific type of diabetes that can develop in some women in late pregnancy (usually after the 24th week).
The test is generally given between 24th and 28th week of pregnancy. However, if you have had gestational diabetes before, or if your doctor is concerned about your risk of developing gestational diabetes, the test maybe performed earlier.
How does a glucose test work?
There are 2 types of glucose screening test.
Two-step testing
- During the first step, you do not need to prepare or change your diet in any way. You will be asked to fast from the night before and drink a liquid that contains glucose in the morning. Your blood will be drawn after that to check your blood glucose level.
- If your blood glucose is too high, you will need to have a second test called a 3-hour glucose tolerance test. To prepare for this test you may only have sips of water for 8 to 14 hours before your test. You will have your blood drawn and then asked to drink a liquid that contains glucose (100 grams). Your blood will be drawn three more times every 60 minutes over a 3-hour period.
One-step testing
- To prepare for this test you may only have sips of water for 8 to 14 hours before your test. You will have your blood drawn and then asked to drink a liquid that contains glucose (75 grams). Your blood will be drawn two more times every 60 minutes over a 2-hour period.
What are the risk factors?
Some women are at a greater risk of developing gestational diabetes than others. The following factors may increase your likelihood of experiencing gestational diabetes:
- A history of high blood pressure
- A history of diabetes in your family
- Being above the age of 35
- Being overweight at the start of your pregnancy – a body mass index (BMI) of 25 or more
- Ethnicity such as African, Native American, Latino, Asian or Pacific Islander
- Gaining an unusually large amount of weight during pregnancy
- Previous complications with pregnancy – gestational diabetes, an unexplained stillbirth or large babies (more than 4kg)
- Personal history of polycystic ovarian syndrome
How can gestational diabetes be treated?
How you are treated for your gestational diabetes will depend on how high your blood sugar levels are.
A change in diet and exercise is generally the most suitable treatment.
For more severe cases, you may be prescribed with oral medication (metformin) or even injectable insulin to regulate your blood sugar levels. These medical treatments are usually only administered until the birth of your child.
Your doctor may also recommend that you use a glucose-monitoring device to check in on your sugar levels.
What are the foods to avoid?
Your doctor and dietitian will advise you to avoid processed food with high sugar content such as:
- Alcoholic drinks
- Processed food with added sugar
- Sweet pastries
- Sugary drinks (fruit juices, energy drinks, sodas)
Diet for a healthy pregnancy and to manage gestational diabetes
To ensure the health of your baby throughout your pregnancy, it is imperative that you manage your gestational diabetes as much as possible. One of the best ways to do this is through proper nutrition. Focus on the proportion of carbohydrates, fat and protein in your daily intake to best regulate your blood sugar levels.
1. Carbohydrates
Carbohydrates fuel your body, providing energy to your cells and your growing baby’s. Emphasise on obtaining adequate calorie for your baby’s growth by including complex carbohydrates in your diet. As a pregnant woman, your carbohydrate (carb) intake should be at least 45% of your calorie intake a day. The rest of your calories should be from protein and fat. Ensure that you eat carbs in controlled portions and evenly distributed over the day to maintain a stable blood sugar level. Divide your carbohydrate load into 3 meals with 2 – 4 snacks throughout the day.
Fibre-rich carbs help blood sugar control by slowing down the absorption of carbohydrates. Examples of these types of food would include:
- Brown rice
- Lentils and legumes
- Oats
- Quinoa
- Wholemeal or whole grains products
It is also important to consume adequate fibre from other sources such as vegetables and fruits to reduce to risk of constipation during pregnancy.
2. Fat
25 – 30% of your calorie consumption should derive from fat. There is a common misconception that fat is bad for our bodies. Although unhealthy in excess, fat is a necessary part of our diet. Essential fatty acids are needed for brain development, inflammation control and blood clotting. They cannot be made by the body and hence need to be sourced from food. Healthy fats like this would include:
- Avocados
- Oily fish
- Seeds
- Unsalted nuts
- Vegetable oil (such as olive oil, canola oil, sunflower oil and etc.)
3. Protein
20 – 25% of calories should be from protein. Proteins are fundamental elements within every cell of the body and are involved in a wide range of metabolic interactions. It is essential for the growth and repair of the body and the maintenance of good health. During pregnancy, proteins positively affects the baby’s growth, including the brain. Good sources of protein include:
- Eggs
- Fish and other seafood
- Legumes and pulses, seeds and nuts
- Milk or milk products
- Poultry, beef, lamb or pork
- Soy products like bean curd and tofu
This guide is only a suggested dietary plan. As a woman with gestational diabetes, you should arrange a consultation with your doctor or dietitian so you can have a dietary plan specialised for you and your lifestyle. Different women have different needs based on their circumstances. Even with gestational diabetes, by eating the right food at the right time, you can still have a healthy pregnancy and a healthy baby.