Cervical cancer is caused by the human papillomavirus (HPV). It is among the top 10 most common cancers affecting women in Singapore.
Prevention is always better than a cure, and in the case of cervical cancer, modern medical advancements have made it much easier to identify warning signs before they develop into something more sinister.
There are two types of tests that can help detect cervical cancer. One is a Pap smear and the other is a HPV test.
In a Pap smear, a tissue sample is taken from the cervix and examined for abnormalities which may indicate cancer. Similarly, in a HPV test, a tissue sample is taken from the cervix and checked for the presence of HPV.
While a Pap smear is the most common form of HPV screening, your doctor may recommend a HPV test if the results from the Pap smear show abnormalities. This offers a better chance of identifying women who are at risk hence a HPV test is recommended for women aged 30 years and above, every 3 – 5 years, depending on your medical history and risk factors for cervical cancer.
Cervical cancer screening for women
Cervical screening is the only routine test for cancers affecting women such as gynaecological precancer and cancer including:
- Cervical cancer
- Uterus cancer
- Ovarian cancer
- Fallopian tubes and vulva
Ovarian cancer, though more deadly, has no effective screening tool to date. As for uterus cancer, it usually presents early with abnormal bleeding, which will alert a woman to seek medical attention.
Where in the past cervical screening was in the form of a Pap smear carried out every 1 - 3 years, doctors now recommend HPV testing as a much more effective method of detecting precancerous changes to the cervix.
Learn more about the common health issues faced by women and how to make the best healthcare decisions.
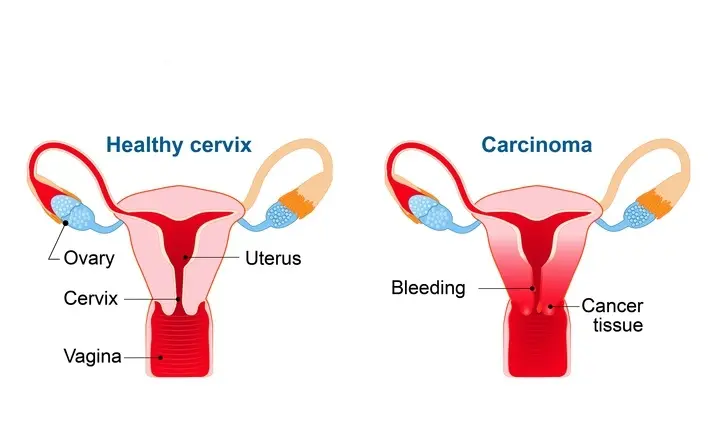
What is cervical cancer?
Cervical cancer is the growth of abnormal cells in the cervix (the lower part of the uterus connecting to the vagina).
It generally develops slowly, but if left undetected, can spread to other parts of the body, such as the vagina, bladder, liver and lungs.
The changes that occur in the tissues of the cervix that lead to the development of cancerous cells are associated with infections of certain strains of the HPV virus.
What is HPV?
HPV stands for human papillomavirus, and is a common infection with over 100 variations or strains.
Many of these strains cause warts on the hands or feet, as the virus lives inside the epithelial cells that are found on the surface of your skin.
However, there are also many types that enter the body via sexual contact, and infect the genital areas, causing genital warts.
Most sexually active adults will contract some form of HPV at some point in their life. Not every strand of HPV is high-risk, but certain types do cause cervical cancer.
Symptoms of HPV
- Many do not experience any symptoms of a HPV infection, and it usually clears up on its own
- Genital warts may appear around the genital area, and are either flat or cauliflower-like lesions that may be itchy but are usually painless
- Common warts are rough bumps on the hands or fingers, and can be painful
- Plantar warts are hard bumps on your feet that may be painful
Why is HPV testing important and why is it done?
Precancerous changes in the cervix occur many years before cancer develops, which leaves a large window of opportunity for screening and detection.
Until recently, the recommended screening test for cervical cancer has always been a regular Pap smear, where cells are taken from your cervix by your gynaecologist or GP and tested for abnormalities.
As this process is subject to sampling and interpretation errors, false negatives can occur, meaning abnormal cells can sometimes go undetected.
HPV testing benefits
HPV testing has proven to be a better screening tool than a Pap smear, and is now recommended for women age 30 and above every 3 – 5 years.
As cervical cancer is caused by high-risk HPV strains, HPV screening offers an even earlier point of intervention. Precancerous changes can be easily treated, and early treatment can not only save a woman's life but also her womb.
What can you expect during the HPV test?
Similar to a Pap smear, a HPV test also collects tissue samples from the cervix hence it is usually performed at the same time, using the same tissue sample.
During the test
Collecting a tissue sample only takes a few minutes. You will need to remove your underwear and lie on an examination table, with your knees bent.
An instrument known as a speculum is then gently inserted into your vagina. It may feel cold at first, and you may feel pressure in your pelvic area as the speculum holds the vaginal walls open. This allows your doctor to collect samples from the cervical wall, using a soft brush and a spatula.
After the test
After the test, you are free to resume your normal daily activities, without any restrictions. You may check with your doctor about when the test results will be available, and make an appointment if one is needed.
HPV test results
The results from your HPV test will be either positive or negative.
Positive HPV test
If your results are positive, it means that you are infected with a HPV strain that is known to cause cervical cancer. A positive result does not mean that you already have cervical cancer. However, it does mean that cervical cancer could develop in the years to come hence your doctor will likely recommend you to take another HPV rest in a year's time. This will show if the infection has cleared or reveal signs of cervical cancer.
Negative HPV test
If your test results are negative, it means that you are not infected with the HPV strains that are associated with cervical cancer.
Next steps
Depending on your test results, some follow-up may be required.
If your test results are negative and your Pap smear results normal, you can continue with the recommended screening schedule.
Sexually active women aged 25 – 29 years are advised to go for a Pap smear once every 1 - 3 years, while those 30 years and above are advised to go for an HPV test once every 3 - 5 years.
If your test results are abnormal, you may be referred to a gynaecologist for several tests. These may include:
- Colposcopy, where a doctor will use a magnifying lens known as a colposcope to examine the cervix more closely.
- Biopsy, in which a sample is taken from the suspected abnormal cervical cells and examined under a microscope. A biopsy may be performed at the same time as a colposcopy.
- Removal of abnormal cervical cells, to prevent them from developing into cancer.
HPV vaccine and immunisation
The HPV vaccine protects against the most common HPV strains that are associated with causing cervical cancer and genital warts.
Types of HPV vaccine
There are currently three HPV vaccines available:
- Gardasil, which protects against HPV 6 and 11, which cause genital warts, and 16 and 18 which are known to cause approximately 70% of cervical cancers.
- Gardasil 9, which protects against HPV 6. 11, 16 and 18, plus the additional HPV strains 31, 33, 45, 52 and 58 which accounts for 10 – 20% of cervical cancer.
- Cervarix, which protect against HPV 16 and 18.
Who should get the HPV vaccine?
The HPV vaccines are approved in Singapore for girls and women aged 9 – 26 years. While it is generally most effective when taken before first sexual exposure, sexually active women may still benefit if they have not been exposed to the strains covered by the vaccine.
Women above 26 years of age may speak to their doctor about their suitability to receive the vaccine.
Those who should not receive the HPV vaccine include:
- Women who are allergic to any of the vaccine components
- Women who are pregnant
- Those who are suffering from an acute infectious disease
- Those who have a bleeding disorder or taking medication that thins the blood
If you have any other questions or concerns about taking the HPV vaccine, speak to your doctor.
Why should you get the HPV vaccine?
As HPV is often sexually acquired, the majority of women are exposed to the virus during their lifetime, and usually in their early 20s.
There are very few cancer vaccines available and the development of the HPV vaccination was a scientific breakthrough. Medical professionals now recommend that all women are vaccinated, and men too, from the age of 9 before any form of sexual activity.
Although the vaccinations do not protect against every strain of HPV, they are almost 100% effective in protecting against the high-risk strains that cause 70% of cervical cancers, and some other cancers too.
How is HPV and abnormal cells in the cervix treated?
If you do have HPV, there are various treatments available to remove the warts and abnormal cells.
- Topical medication can be applied to warts to remove them from the skin
- Cryotherapy is a process where the warts are frozen off with liquid nitrogen
- Electrocautery is a process where the warts are burned off with an electric current
- Laser surgery or standard surgical removals are also options to remove abnormal cells
Prevention
The HPV vaccine is available at Gleneagles Hospital and Parkway Shenton clinics. It is also available for free under the school-based vaccination programme, for Secondary 1 female students.
Eligible women aged 9 – 26 years old may use up to $500 – $700 per Medisave account, per year, to receive either Cervarix or Gardasil. Immediate family members, such as parents or spouses, may also use their Medisave to cover the cost of the vaccine.
Patients eligible for the Community Health Assist Scheme (CHAS) may receive the Cervarix (HPV2) vaccine in CHAS-accredited Parkway Shenton clinics only at $90/dose (subject to eligibility). Simply walk in to our dedicated vaccination clinic at Esplanade MRT or call any of our clinics islandwide to confirm the availability of your preferred vaccine.
While the HPV vaccine offers excellent protection, regular visits with your gynaecologist and following their screening recommendations are essential for staying on top of your health. Even if you are vaccinated, cervical cancer screening remains the best way to detect any issues early.