If your knees are in constant severe pain, and walking is a struggle, there's a chance you may one day need knee replacement surgery.
What is knee arthroplasty?
Knee arthroplasty is essentially the replacement of part of your knee by an orthopaedic surgeon. The damaged part of your knee is removed, and an artificial joint made of plastic or metal is inserted and attached to the existing structures in your knee. Usually this surgery is performed under general anaesthetic.
Types of knee replacement surgery:
- Total knee replacement, which usually means replacing the entire joint surfaces at the end of your thigh bone (femur) and shin bone (tibia), and sometimes replacing the structure under your kneecap.
- Partial knee replacement, which is a good option if only part of your knee is affected. It involves replacing specific damaged sections of the knee, and means faster recovery and better function.
- Knee cap replacement, which is suitable if the patella and the corresponding part of the femur bone are the only parts of the knee that are affected. However, this surgery may not be recommended often as not many people experience wear and tear in this area alone.
- Complex knee replacement, performed when the condition of the knee is extremely poor, or to repair a previous replacement surgery.
Why would you need knee arthroplasty?
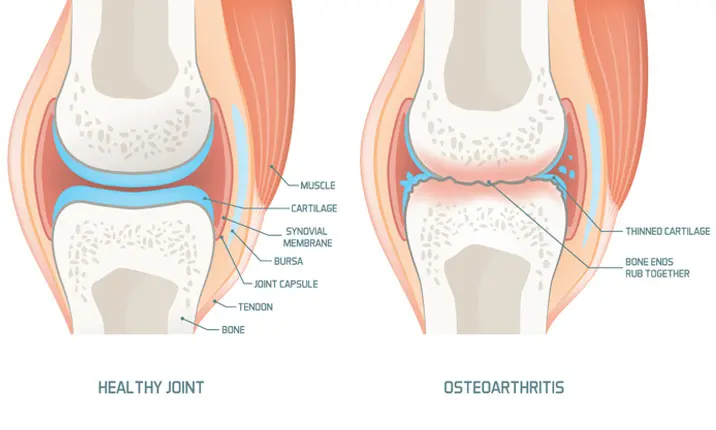
The most common reason for knee replacement surgery is arthritis. Arthritis comes in many forms but broadly covers diseases affecting the joints. Knee osteoarthritis is caused by wear and tear of the cartilage, which is the layer that absorbs shock and helps the joint move smoothly. When the cartilage at the knee breaks down, it results in swelling, stiffness and pain. When knee osteoarthritis becomes severe, the sufferer may become almost immobile.
Other less common reasons for needing a knee replacement include:
- Gout, a condition that results when crystals form at the joint
- Ligament damage or injury, leading to increased knee degeneration
- Haemophilia, a blood clotting disorder
- Necrosis, or death of the bone
- Bone dysplasia, a bone growth disorder
Alternatives to surgery
Surgery is not something to be taken lightly, so your doctor will encourage you to consider alternatives before choosing to undergo knee arthroplasty. Some common options include:
- Weight loss, which will reduce strain on your joints, strengthen muscles and ease pain
- Physiotherapy, which can involve specialised exercises to strengthen your joints, as well as ultrasound or electrical therapy
- Injections of hyaluronic acid to lubricate the joint and ease pain
- Injections of cortisone to reduce inflammation
- Medications such as topical creams
- New or novel treatment options like platelet-rich plasma injections. However, more research is required in this area before it can be recommended as a standard form of treatment.
- Minor surgery like arthroscopy, which is the removal of bone fragments
Preparing for and recovering from surgery
If you and your doctor decide surgery is the best option for you, here's what to expect.
Pre-surgery, you'll be required to undergo a full examination, which will include scans, such as x-rays, to view the full extent of damage to your knee. If you are obese, you may be required to lose weight. Your medical history will also be taken into consideration. Any pre-existing medical conditions will need to be properly controlled and optimised.
If the surgery goes ahead, you may experience discomfort and stiffness when you wake up. However, with modern methods of pain relief, you'll probably find this bearable and be able to start physical therapy the day after. Early commencement of physical therapy is helpful to encourage blood flow to the surrounding tissues. You might need a walking aid, crutches or a stick for a while, but you should see a big improvement in flexibility and pain levels after 6 weeks of surgery. Your doctor will work with you to decide on the best physical therapy schedule for your recovery, based on the type of surgery you had and your overall health.
Remember:
- Staying mobile will greatly help to speed up recovery
- Icing and elevating your knee can ease inflammation
- Continue to take any medication prescribed by your doctor
- Your doctor may have you wear a compression garment to promote blood flow
- You may be able to drive a few weeks after surgery, but if you are still on medication that might hinder your judgement, you should not drive even if your knee feels better. Always check with your doctor.
- If you travel in the weeks after your surgery, make sure you stay mobile to reduce your risk of blood clots
Complications and risks
As with any surgical procedure, there are risks. Some of these risks include side effects from anaesthesia, such as vomiting, nausea, pain and drowsiness. Blood clots are another potential complication, which can form during surgery or in the weeks after, as your body assumes the clotting process at the wound site. If a clot moves to your heart or lungs it can be fatal, so talk to your doctor about ways to prevent this. Your doctor would also be on the lookout for signs of infection at the wound, such as:
- Bleeding complications
- A buildup of fluid which might need draining
- Skin not healing properly
- Fever or chills
- Coloured discharge from the wound that smells
- Increased redness around the wound
If you notice any of the above symptoms, or if you are concerned about the way you are healing from surgery, speak to your doctor immediately.
So, do you need knee replacement surgery?
If you suspect you may need knee arthroplasty, see a specialist for a consultation. There may be steps you can take, before resorting to surgery, to ease your pain and symptoms. Otherwise, your doctor will advise the best treatment or surgery for you to ensure you have the best possible outcome.
People who suffer from severe joint pain often find that knee replacement surgery is life-changing, so if it's right for you, it can make a big difference to your quality of life.