Kneecap, or patella, dislocation in children happens more often than we think. In Singapore, statistics obtained by The National University Hospital (NUH) show that there are approximately 100 cases of young patients who experience kneecap dislocations every year.
A dislocated kneecap usually happens when a child falls, or takes a hit to the knee. Typical scenarios include playing contact sports such as soccer. Symptoms may vary from each patient leaving you confused as to how to proceed.
Read on to understand more about dislocated kneecaps, the symptoms, and what needs to be done when they do happen.
What is a kneecap dislocation?
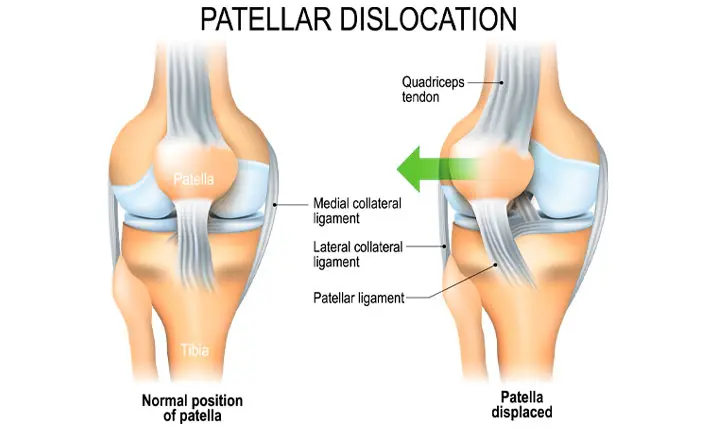
The kneecap, also known as the patella, is a triangular bone that forms part of the knee joint. The patella rests in a groove located at the end of the thighbone (femur). When you move your knee, the patella slides up and down within the groove and facilitates movement. As long as your patella is correctly placed in the groove, walking, running and moving about happens naturally.
But should a fall, or a hard blow to the knee happen during sports, the patella may slip out of place and get dislocated. It can be a partial or complete dislocation that is accompanied by pain and mobility issues.
What are the symptoms?
The symptoms your child may experience will depend on the extent to which the patella is dislocated, and the amount of damage sustained.
Here are some of the commonly experienced symptoms:
- Pain, swelling and discomfort
- Popping sound as the patella dislocates
- A sensation that the patella has shifted
- Deformed or misshaped knee
- Inability to walk or straighten the knee
Who is at risk of a dislocated knee?
Almost 60 – 80% of kneecap injuries usually occur when performing a cutting/turning action while the foot is firmly planted on the ground. These can be common in children active in sports such as basketball, soccer, and rugby. Teenagers participating in gymnastics and dancing are also at high risk. A direct blow to the knee can also cause kneecap dislocation, though this happens less frequently.
Apart from these, inborn deformities of the thighbone, kneecap and ligamentous laxity can make your child more prone to this injury. It’s also common in children with a family history of knee instability. Unfortunately, such deformities cannot be corrected without surgery.
How is the condition diagnosed?
The doctor will first conduct a thorough medical history, to assess the mechanism of injury and symptoms your child is experiencing. Next, a physical examination is performed to check for the range of motion, swelling, and deformity if any. The doctor needs to assess if the patella is still dislocated or if the swelling has been reduced.
He will also order imaging tests such as X-rays and magnetic resonance imaging (MRI) scans which will help in assessing the extent of injury. These will help decide on the treatment plan.
What are the treatment options?
The treatment options are guided by the extent of injury.
1. Immediate treatment
If you feel that your child’s knee is out of place, take your child immediately to the Urgent Care Centre (UCC). The doctor may return the kneecap to its proper place by a process called "Manipulation and Reduction". Analgesia and sedation may be required in order for the doctor to perform this.
2. Non-surgical treatment
Non-surgical treatment options involve immobilisation by use of a knee brace and crutches, rest, ice, compression, and elevation. Physiotherapy and rehabilitation may also be suggested. The doctor may also prescribe medication in order to control the pain and swelling.
3. Surgical treatment
Surgery is required if the patella dislocates multiple times, continues to be unstable despite treatment, or if there's evidence of bone injury. The type of surgery required is guided by the injury sustained as well as the root cause. Damaged tissue such as ligaments are repaired or reconstructed and the occasional bone procedure may be warranted. These can often be performed via a minimally invasive approach. Bony injuries are treated with a lower threshold for surgery as there’s an increased risk of arthritis setting in.
How can you reduce the risk of kneecap dislocations in children?
Some of the ways we can help reduce the risk of this occurring again include educating the child on what positions can lead to it and how to avoid them. Physiotherapy to strengthen the relevant muscles are another way of reducing the risk of the injury occurring. These are important as recurrent dislocations lead to structural damage and subsequent development of arthritis.
When do you see a paediatric orthopaedist?
If you suspect your child of having sustained this injury, consult a doctor as soon as possible. This is especially if the patella remains dislocated as evidenced by your child complaining of inability to move the knee, or bear weight. You are advised to see a paediatric orthopaedic surgeon immediately.
To avoid future recurrence, you should ensure that your child is familiar with the at-risk positions and activities and muscle-strengthening exercises.
What should you take note of post-recovery?
Conservative management usually follows the RICE method which involves 4 steps – Rest, Icing, Compression, and Elevation. This usually takes 3 – 6 weeks, but can sometimes extend up to 3 months or more, depending on the extent of injury.
The timeline of recovery from surgical management is somewhat similar. Skin wounds take 2 weeks to heal, but soft tissue and bone surgery procedures may take up to 3 months and more. However, one should be aware that injuries in children tend to heal a lot faster than adults.
Resumption of normal activities is dependent on the course of action as well as the progress in healing. The doctor assesses each patient individually, but most patients are fit to return to sporting activities within 3 – 6 months, once full range of movement and strength is demonstrated.