COVID-19 has drastically affected our lives over the last two years. Thankfully, the high vaccinations rates here in Singapore have given us a significant degree of protection as our country begins to open up and treat COVID-19 as endemic.
As of 21 May 2023, data from the Ministry of Health’s (MOH) website shows that about 89% of Singapore’s total population have completed the primary vaccination series.
But while COVID-19 infections may be commonplace, and vaccinated individuals have significant protection against serious illness and hospitalisation, the virus should not be brushed off as mild. Neither should its potential risks to one’s long-term well-being be dismissed. Safety precautions such as mask wearing and keeping our hands clean should still be taken as COVID-19 can affect everyone differently.
A case in point is what’s been described as long COVID, whereby an individual continues to experience lingering symptoms such as fatigue and breathing difficulties, long after recovering from the initial COVID-19 infection.
Dr Adrian Chan, respiratory physician and intensivist at Mount Elizabeth Novena Hospital, shares more about long COVID by highlighting some of the key symptoms, the possible effects on the body, risk factors to watch for, and how it can be managed.
Tell us more about long COVID. What are the symptoms to look out for and how long do they typically last?
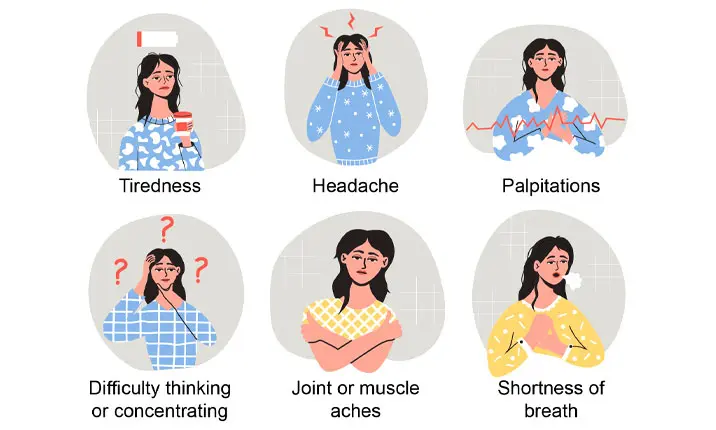
Long COVID can manifest in many ways. According to US Centers for Disease Control and Prevention (CDC), these symptoms can include:
- Shortness of breath, especially on exertion
- Tiredness
- Difficulty thinking or concentrating (“brain fog”)
- Cough
- Chest or stomach pain
- Headache
- Palpitations
- Joint or muscle aches
- Pins-and-needles feeling in the limbs
- Diarrhoea
- Sleep problems
- Dizziness on standing (light-headedness)
These symptoms can last for weeks to months.
How prevalent is long COVID among our population? Are fully-vaccinated individuals (those who have completed their primary series of vaccination and received booster shots) less likely to develop long COVID?
About one in 10 people report some symptoms up to six months after recovering from a COVID-19 infection.
The best way to prevent long COVID is to avoid getting infected in the first place, and this is well-achieved with COVID vaccination. Compared to unvaccinated individuals, the risk of developing long COVID could be reduced by half in vaccinated individuals.
Is there a scientific reason for why some people get long COVID, while others recover fully?
There is currently no established explanation or theory as to why some patients are susceptible to getting long COVID. Some hypotheses that have been put forward include virus-specific pathologic changes or immunologic reactions following the initial infection. As COVID is a relatively new illness, there are ongoing studies to study the long-term physical and psychological aspects of COVID.
Are there any risk factors for long COVID that we should be aware of?
Some risk factors that have been reported include older age, female gender, pre-existing chronic medical conditions such as hypertension or obesity, and initial severe acute COVID-19 illness.
Beyond the initial infection, how does the COVID-19 virus affect our body functions and lead to chronic health problems?
The COVID-19 virus can damage the lungs by increasing the inflammation in the airways and lung tissue.
This is especially so in patients who contracted COVID bronchitis and/or pneumonia initially. Even after the patient recovers, the inflammation may persist, resulting in prolonged symptoms such as breathlessness, cough, and sputum production.
As these symptoms tend to persist over time, when should COVID-19 patients seek help from a doctor?
It is advisable for patients who have persistent symptoms or develop new or worsening symptoms after recovery from COVID-19 to see a specialist for a medical evaluation to help ensure a smoother recovery, especially for those patients with prolonged or significant symptoms of breathlessness, cough, chest pain, and palpitations.
What can these patients expect during their specialist consultation?
The specialist will take a detailed history of their long COVID symptoms and perform a thorough physical examination.
Depending on the symptom presentation, further investigations such as blood tests, chest imaging, lung function testing, electrocardiogram, echocardiogram, and dynamic exercise testing may be conducted.
How would their symptoms be treated or managed?
The goal of medical management is to optimise function and quality of life during the period of symptoms as the patient gradually recovers.
For example, being breathless does not mean that the patient should just adopt a sedentary lifestyle. Rather, the patient should be guided on improving his/her breathing and tailoring the exercises as he/she returns to fitness.
Can you share any interesting observations about COVID-19 patients in your practice as a respiratory specialist?
Most patients who consult for respiratory symptoms following recovery from COVID-19 may face discomforting and prolonged symptoms, but otherwise, they are able to carry on with their basic daily activities.
A personal observation is that some patients do find it takes a while to recover exercise capacity, even if basic lung function testing and radiologic imaging prove to be normal.
Do you have any recovery tips for patients with long COVID?
Experiencing post-COVID symptoms can be distressing and frustrating, especially if the symptoms become prolonged. Discuss with your loved ones and seek medical attention to share your symptoms and formulate coping strategies. Improve your health by adopting healthy living habits, such as gradually resuming exercise, getting sufficient sleep, and eating well.
Should parents be concerned about their children getting affected by long COVID?
A person of any age who has had COVID-19 can go on to develop a post-COVID condition. This includes both adults and children. Fortunately, current data suggests that post-COVID conditions appear to be less common in children and adolescents than in adults.
Symptoms of post-COVID in children and adolescents are similar to those in adults. However, as younger children may have difficulty in describing the symptoms they are experiencing, parents should remain observant and aware of the signs of long COVID when interacting with their children.