For some of us, a COVID-19 infection can hit us hard with intense symptoms that take days or even weeks to fully recover from. But what if some of the symptoms persist even after you have recovered from the initial COVID-19 infection?
"Long COVID" is a term used to describe the presence of various symptoms, weeks to months after being infected with COVID-19. Dr Serene Wee, general practitioner at Parkway Shenton Medical Clinic at Robinson Road, answers some common questions about long-COVID and the symptoms to look out for so you can get the help you need.
What are some of the factors that make you susceptible to long COVID?
Risk factors for long COVID include:
- Being female
- Being older in age
- Having experienced more than 5 symptoms during the acute stage of a COVID-19 infection
- Presence of comorbidities such as heart or lung disease
What are the stages of long COVID?
Long COVID can be classified into 2 stages:
| Stage | Symptoms |
|---|---|
| Stage 1: Post-acute COVID | Extends beyond 3 weeks, but less than 12 weeks |
| Stage 2: Chronic COVID | Extends beyond 12 weeks |
Does everyone with long COVID experience the same symptoms?
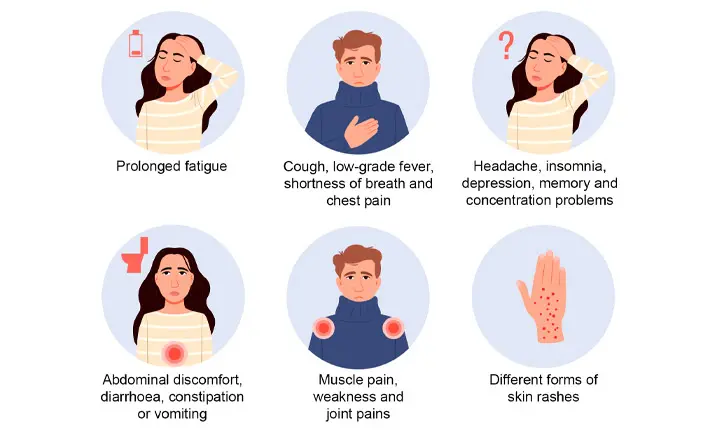
No, long COVID can be experienced by different people in different ways. Here are some types of long COVID syndromes and their accompanying symptoms.
| Long COVID Syndromes | Symptoms |
|---|---|
| Post-COVID fatigue syndrome | Profound fatigue |
| Post-COVID cardio-respiratory syndrome | Cough, low-grade fever, shortness of breath and chest pain |
| Post-COVID neuro-psychiatric syndrome | Headache, insomnia, depression, memory and concentration problems |
| Post-COVID gastro-intestinal syndrome | Abdominal discomfort, diarrhoea, constipation or vomiting |
| Post-COVID musculoskeletal syndrome | Muscle pain, weakness and joint pains |
| Post-COVID dermatological syndrome | Different forms of skin rashes |
More serious symptoms of long COVID can include deranged liver enzymes, jaundice, pulmonary embolism (a blockage in a pulmonary artery) in the lungs and kidney injuries.
How is long COVID determined in a patient?
| Symptoms | Diagnostic tests |
|---|---|
| For all patients with long COVID | Routine laboratory assessments should be conducted. They include: * Complete blood count. * Comprehensive metabolic panel that includes testing for renal and liver function. * Coagulation panel – a test that identifies problems with your blood's ability to clot, and the duration taken for your blood to clot. * If clinically indicated, other tests can be conducted such as: * C-reactive protein (CRP) – tests the inflammation in your blood and can evaluate risk of heart disease. * Fibrinogen – tests the level of this blood plasma protein that contributes to blood clotting. * D-dimer – helps determine the presence of a serious blood clot. * Troponin – helps determine if you are having a heart attack. * Ferritin – helps determine if you have iron deficiency. |
| For patients with respiratory symptoms | * Repeat pulmonary imaging, preferably with a high-resolution computerised tomography scan (HRCT) or computerised tomography angiogram. * Heart function tests such as electrocardiogram and echocardiography must also be considered to rule out an underlying cardiopulmonary disease. |
| For patients with neuropsychiatric manifestations. | * Neuroimaging that includes vascular and neuropsychological testing such as the computerised tomography (CT) or magnetic resonance imaging (MRI) must be performed. |
How can long COVID be managed?
Long COVID can be considered a multi-system disorder that results in respiratory, cardiovascular, hematologic, and neuropsychiatry symptoms either alone or in combination.
Care for the condition should address the clinical and psychological aspects of this disorder by incorporating a holistic and inter-disciplinary approach involving the below specialties and specialists:
- Primary care
- Respiratory medicine
- Cardiology
- Infectious disease
- Psychiatrists
- Psychologists
- Physical and Occupational therapists
- Social workers
Should you face concerning symptoms such as the below, seek medical attention from the following specialists and learn about the potential evaluations and treatments you may be advised to undergo:
| Symptoms | Specialist | Evaluation/ Treatment |
|---|---|---|
| Persistent or residual pulmonary symptoms | To be seen by a respiratory physician as early as possible for evaluation and follow-up | * Enrolment into a pulmonary rehabilitation program, which is key for faster clinical recovery * Vaccination against influenza and streptococcus pneumoniae (a cause of community-acquired pneumonia) should be given. * Pulmonary function tests like spirometry and computed tomography (CT) chest should be considered if clinically indicated as well. |
| Patients who continue to have persistent cardiac symptoms after recovery from COVID-19 | To be monitored by a cardiologist | * To rule out arrhythmias, heart failure, and ischemic heart disease, cardiac function tests should be conducted such as an: * Electrocardiogram * Echocardiography * If clinically indicated, an MRI of the heart should be ordered, given the increased incidence of myocarditis or inflammation of the heart muscle in patients with COVID-19. The MRI will evaluate the following: * Myocardial fibrosis - where there is an increase in the volume of collagen in the myocardial * Scarring of the heart muscle |
| Anxiety, depression, insomnia, post-traumatic stress disorder | Psychiatrist or Psychologist | * Patients should be screened for common psychological issues and referred to a psychiatrist or psychologist if so advised. |
As long COVID continues to be a concern among those infected with COVID-19, be mindful that persistent symptoms or new or worsening symptoms ought to be checked out by a medical professional so you can get started on a suitable treatment plan promptly.
Think you may be facing long COVID or know someone who might be?
Locate the nearest Parkway Shenton clinic to you here and make an appointment for a medical evaluation.