In October 2018, Britain's Princess Eugenie made news the world over for her choice of wedding gown. Not because the dress was haute couture, but because it showcased a long scar running down her back, the result of a spinal surgery she had as a child. Interestingly, she chose to wear her scar with pride so as to honour the medical professionals who had helped her, and to inspire other patients with scoliosis (curvature of the spine).
Unlike Princess Eugenie, however, not everyone wants to have their scars on show. In fact, many patients prefer not to be left with any obvious scars after their surgery.
Thanks to technological advances these days, patients who require certain spinal surgeries can either go for traditional open surgery or opt for minimally invasive spine surgery (MISS), a newer approach that leaves less noticeable scars and offers a shorter recovery time.
What is open spine surgery?
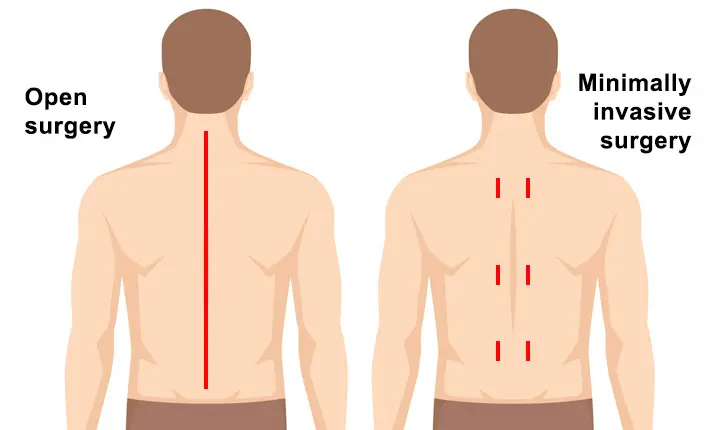
Traditionally, spine surgery is performed as 'open surgery', meaning that the surgeon makes a long incision along the patient's back, and cuts and retracts any surrounding muscles to access the spine. Then, depending on the type of procedure, the surgeon proceeds to remove any damaged bone or intervertebral discs, or place screws, cages and bone graft materials necessary to stabilise the spine. Once the surgery is complete, the long incision is sutured up and left to heal, which could take up to several months.
Benefits of open spine surgery
Some studies indicate that open spine surgery leads to better outcomes in treating certain spinal conditions such as cervical and lumbar disc herniation.
Risks of open spine surgery
Open spine surgery normally involves a single, larger incision and more damage to the tissues and muscles. This in turn will likely lead to more pain after surgery and a longer recovery time.
Apart from these, any kind of surgery involves risks which may include:
- Blood clots in the legs, known as deep vein thrombosis
- Infection
- Blood loss
- Injury to the spinal cord
What is minimally invasive spine surgery?
Comparatively, minimally invasive spine surgery is a more localised procedure. In this procedure, the surgeon relies extensively on image guidance technology such as pre- and intraoperative 3D imaging, fluoroscopy, CAT scans and intraoperative navigation to plan the surgical approach. The surgeon begins by making small incision(s) directly over the pathological area(s). Then, special retractors are used to help dilate soft tissues and move muscles out of the way, instead of dissecting them like in open surgery. At the end of surgery, sutures are placed to repair the small incision(s).
Benefits of minimally invasive spine surgery
Dr Yue sums up some benefits of minimally invasive spine surgery:
- Produces similar long-term results as open spine surgery.
- Smaller scars, usually only 2 inches or less, whereas open surgery scars are typically 5 – 6 inches long.
- Less blood loss and collateral damage to surrounding tissues.
- Reduced risk of post-operative complications.
- Less likely to develop infection at the surgical site compared to patients who had undergone open surgery.
- Shorter hospital stay, smoother recovery process and faster return to normal activity.
In fact, a study published by Dr Yue in 2013 found that for patients who had undergone transforaminal lumbar interbody fusion (TLIF), a surgery that stabilises the spine by creating a solid bridge of bone between spinal bones, those who opted for MISS:
- Experienced about 3 times less blood loss during the operation
- Required close to 4 times less painkillers on average after the operation
- Were confined to bed for only half the usual time needed
- Were hospitalised for around half the duration compared to open surgery patients
- Shared similar longer-term results as open surgery patients when observed over a 5-year period
In addition, a surgeon's familiarity with the procedure also plays an important role. In a study conducted by Dr Yue between 2005 and 2009, proficiency in minimally invasive spinal procedures such as transforaminal lumbar interbody fusion (TLIF) can only be achieved for most surgeons after 44 operations.
Risks of minimally invasive spine surgery
Any form of surgery comes with risks, even if it is a minimally invasive procedure. However, as it involves smaller incisions, the risks of blood loss, infection, tissue and muscle damage are reduced.
Overall, minimally invasive spine surgery is also relatively newer procedure compared to open spine surgery, hence its use in more rare and complex spinal conditions is still being researched.
Which is better – Minimally invasive spine surgery or open surgery for the spine?
While minimally invasive spine surgery does present many benefits, bear in mind that it is not for everyone. Your doctor will recommend a suitable procedure based on the spine condition being treated, your health and other considerations.
Minimally invasive spine surgery procedure
While the operation may vary depending on the condition that is being treated, a minimally invasive spine surgery will generally include:
- General anaesthesia which will put you to sleep for the duration of the procedure, or localised anaesthesia and sedation which allows you to remain conscious.
- Careful monitoring of your heart rate, blood pressure and other vital signs.
- While lying face-down on the operating table, your surgeon will make one or more small incisions in your back to access the area that needs treatment. The incision will be held open with a tubular retractor.
- Specially modified surgical tools will be inserted for the surgeon to perform the treatment. A powerful operating microscope or a small camera and light may be inserted; to allow the surgeon to see the anatomy and tools clearly.
- The incision or incisions will be closed with sutures and dressed.
If you have any questions about undergoing spinal surgery, read more about it here.
If you're considering spinal surgery, do consult your surgeon to discuss the treatment options available and how you can benefit from the procedure.