Scars form as part of the healing process when your skin gets damaged. Once your skin is damaged, the scar that is left is permanent, although it may fade with time. Scars in prominent anatomical locations such as the face and hands may lead to significant functional and social embarrassment, while scars in other locations may cause bothersome symptoms such as itch, pain and limitation of movement.
What causes scars?
The type of scar, its appearance and its treatment depend on several factors including:
- depth of the wound
- size of the wound
- age
- ethnicity
- gender
- genes
Are all scars the same?
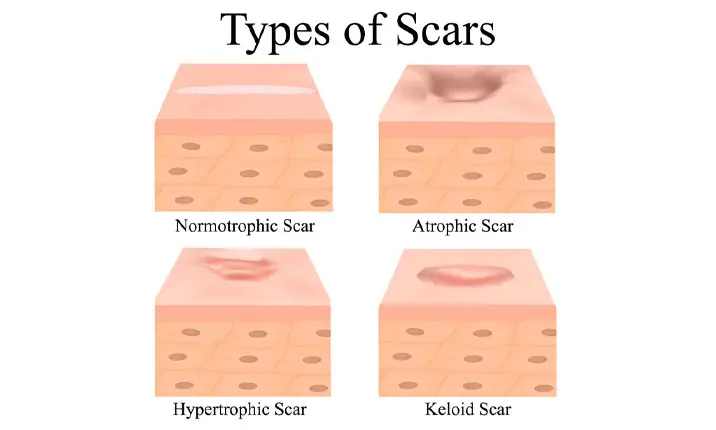
There are various types of scars and which type you have will depend on the type of injury to the skin.
Keloid scars: These are raised scars, most common among people with dark skin. Genetic factors result in the skin healing over-aggressively. Depending on their size and location, the scars can affect your movement. These scars can be prevented from forming as the skin heals with the use of silicone gels or sheets, pressure garments and steroid injections.
Hypertrophic scars: These are red and raised, similar to keloid scars, but remain within the boundary of the injury.
Acne scars: Severe acne can lead to pitted scarring and treatment depends on the type and severity.
Contracture scars: These are the result of burns that tighten the skin and can impair movement at joints. They can also be very deep, affecting the muscles, tendons and nerves under the skin.
How can scarring be prevented?
The obvious way to prevent scarring is to avoid injury by wearing protective equipment such as pads or guards during activities such as cycling or rollerblading, when there is a risk of injury. Where there's an injury, having a professional attend to the wound with measures such as stitches and draining of the wound, can minimise the potential of scar formation. After the wounds have healed, meticulous post-injury wound care is important to further minimise the severity of scarring.
Examples of precautions you can take during the healing process include:
- covering the wound with a bandage to prevent re-injury or infection.
- using silicone covering to improve the skin's appearance.
- avoiding picking at scabs, which can introduce bacteria and cause infection. Let them crust and fall off naturally. To reduce scarring after the scab falls, keep the tender pink skin covered as it heals.
- getting stitches if the wound is deep or wide, and following your doctor's instructions on managing the stitches.
Should I treat burns differently?
You can take extra precautions to minimise scarring from minor burns as soon as the accident happens by following the measures below:
- Rinse the area under cool water and let it air dry.
- Apply antibiotic cream with a sterile tongue depressor to avoid introducing bacteria into the wound.
- Apply a non-stick bandage onto the wound.
- Stretch the area daily to avoid the skin tightening after the wounds have healed.
- Blisters are a natural part of the healing process, but resist the urge to pop them as this can introduce bacteria into the wound. De-blistering of burn injuries by trained professionals have been shown to reduce the potential of wound infection.
- Keep the injured area away from direct exposure to the sun.
Can my scars be treated?
To lessen the appearance of scars, there are treatments your dermatologist or plastic surgeon may recommend depending on the characteristic of scarring.
Dermabrasion: As long as you don't have sensitive skin or any autoimmune disorders, this exfoliating treatment may be an option. Dermabrasion uses physical techniques to remove the top layer of the scar and stimulate skin renewal, improving the size and shape of the scar.
Cryotherapy: Used in the treatment of keloid and hypertrophic scars, this method involves freezing the scar with nitrogen vapour. The treated area will turn red and possibly blister after the treatment. The treated area will form a scab, which usually heals in 1 – 3 weeks.
Chemical peels: This is a common treatment for acne scars. It removes the outer layer of the scar and, as the skin repairs itself over around 14 days, it usually grows back smoother. Your dermatologist or plastic surgeon may also treat acne scarring with collagen or similar fillers, but this is usually not seen as a permanent solution.
Laser therapy: Laser therapy is similar to a chemical peel but involves a concentrated beam of light to remove the outer layer of the scar. Recovery is quicker than with a chemical peel, at 3 – 10 days.
Steroid injection: Steroid injections are one of the most effective and reliable methods of scar treatment. This treatment is suitable for keloid and hypertrophic scars. Your doctor will inject a corticosteroid into your scar to flatten and soften raised and firm scars.
Fat grafting: Depressed scars are suitable for treatment with fat grafting. This is a minor surgical procedure performed under local anaesthesia and fat is harvested from the abdomen, inner thighs or hips through small incisions and then grafted into depressed scars. Fat grafting provides permanent improvement to the appearance of the scar.
Surgical removal: Scars that benefit from surgical removal are those that are painful, occupy a large area, cause limitation of joint movement or are unresponsive to other forms of treatment. Depending on the extent of surgery required, this may be performed under local anaesthesia or general anaesthesia, often as a day surgical procedure.
Should I worry if a wound is slow to heal?
Minor wounds may often be treated by simple over-the-counter remedies, whereas large wounds, deep wounds and burn wounds will benefit from immediate medical attention.
Once your skin is injured, it will go through its natural stages of healing. You may experience swelling, pain, redness or notice a clear discharge in the first week. See a doctor if any of these symptoms get worse or last longer than a week.
As the wound starts to heal, new tissue will grow over it and the full healing process can take 2 weeks. The following symptoms are signs that your wound is not healing as it should:
- Persistent fluid or pus drainage from the wound
- Redness and warmth around the wound, especially if it spreads
- Bad odour coming from the wound
- Worsening pain
- Skin becoming dark at the wound edges
- Fever
Should you encounter any of the above warning signs when your wound is slow to heal, visit the Urgent Care Centre (UCC) immediately.