Fibroids and cysts affect different structures within a woman's reproductive system. However, they can both present with similar symptoms, such as pelvic pain and abnormal uterine bleeding. There's also a possibility that both conditions can affect fertility.
Fibroids affect the uterus while cysts occur in the ovaries. Treatment depends on the symptoms, plans for a family, and can take the form of non-surgical as well as surgical intervention. Both fibroids and cysts are diagnosed by an ultrasound scan.
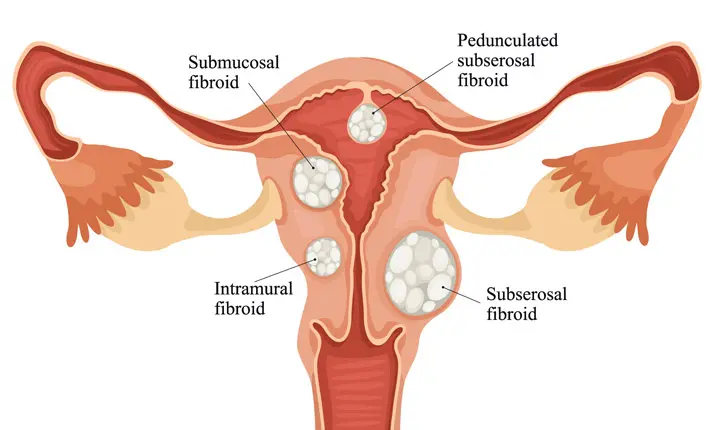
What are uterine fibroids?
Uterine fibroids are non-cancerous muscular growths within the walls of the uterus. They can grow up to several centimetres in diameter, but are often undetected because they don't cause any obvious symptoms. Fibroids are very common and around 50% of all women will have fibroids by the time they reach 50. These are usually detected during their routine gynaecological examinations. Fortunately, most women that have small fibroids have no symptoms. On average, only 25% of women will ever experience symptoms.
What are the symptoms of fibroids?
You might have fibroids in your uterus if you experience the following symptoms:
- Heavy and painful periods
- Abnormal uterine bleeding
- Abdominal and pelvic cramping
- Lower back pain
- Pain or pressure during intercourse
- Frequent or difficulty passing urine
When in doubt, consult your gynaecologist as fibroids can complicate a pregnancy and can lead to miscarriage and/or infertility.
What are the causes of fibroids?
The exact cause of uterine fibroids is not known, but they have been linked to:
- Oestrogen and progesterone, hormones which stimulate the development of the uterine lining during each menstrual cycle. Fibroids contain more of these hormone receptors than other muscles in the uterus, and the decrease in hormone production during menopause sometimes causes fibroids to shrink.
- Pregnancy, which increases the production of oestrogen and progesterone
- Family history of fibroids, especially among close relatives like your mother or sister
Other factors which may increase your risk for developing fibroids are:
- Obesity
- Diet high in red meat and low in vegetables, fruit and dairy products
- Alcohol consumption
- Vitamin D deficiency
- Early onset of menstruation
Overall, a family history of uterine fibroids could indicate a risk for the condition, but maintaining a healthy lifestyle and weight can reduce a woman's risk of developing fibroids.
How are fibroids treated?
The treatment plan for fibroids will depend on how the symptoms are affecting your daily life, your body's ability to function normally, and whether you plan to have children.
Fibroids can impact your fertility
While many women with fibroids do not face fertility issues and have successful pregnancies, some fibroids can cause inflammation of the uterine lining and change its local hormonal environment, affecting the implantation of the embryo.
If the fibroids get too large, it can result in changes in the shape of the cervix, which can affect the number of sperm that can enter the uterus or interfere with the movement of the sperm or embryo. Fibroids also can block the fallopian tubes, making conception difficult.
Medication
Your gynaecologist may adopt a watch-and-wait approach to see if medication can relieve your symptoms.
Hormonal medication may be prescribed to regulate your menstrual cycle and reduce the pain and heavy bleeding. They can also arrest the growth of fibroids.
Treating fibroids if you are trying to conceive
If you are planning to conceive, medication may be prescribed to help shrink the fibroids or a procedure known as a myomectomy may be recommended to remove them.
It may also help to make some lifestyle changes such as avoiding high-calorie foods, reducing your intake of meat, and increasing your intake of green vegetables and fish such as tuna or salmon. Losing weight and managing your stress levels may also help.
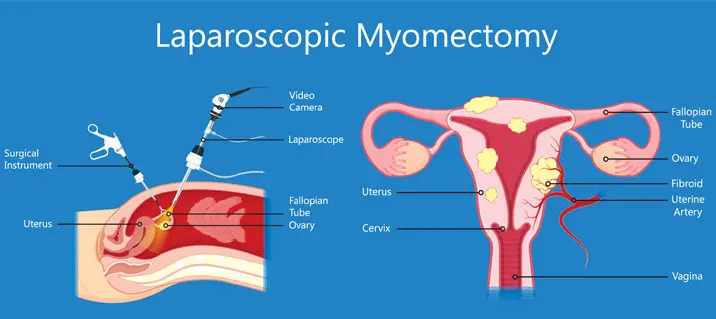
Myomectomy to remove fibroids
A myomectomy is a procedure to remove fibroids from the uterus without removing the uterus itself.
This makes it possible for women to conceive in the future.
It can be performed in different ways:
- Abdominal myomectomy, in which the fibroids are removed through an open surgical cut in the abdomen.
- Laparoscopic myomectomy, which removes fibroids through several small incisions. It is less invasive than an abdominal myomectomy, with a shorter recovery time.
- Hysteroscopic myomectomy, otherwise known as Transcervical Resection of Myoma (TCRM), uses a special scope to remove fibroids through the vagina and cervix.
Treating fibroids if you are not trying to conceive
If pregnancy is not a concern or if you are not planning to conceive, your gynaecologist may recommend a uterine artery embolization (UAE), an MRI-focused ultrasound therapy or a hysterectomy instead.
These procedures are usually not recommended for those who wish to conceive, which is why you should speak to your doctor in detail about the possible risks involved.
Uterine artery embolisation (UAE)
In a uterine artery embolisation (UAE), fibroids are destroyed by cutting off their blood supply.
MRI-focused ultrasound therapy
MRI-focused ultrasound therapy is a non-surgical technique that destroys the fibroids with high-intensity ultrasound waves.
Hysterectomy
As a definitive end to symptoms, you could elect to have a hysterectomy, where the uterus is removed but the ovaries, which are responsible for producing female reproductive hormones, are kept in place so that you do not enter early menopause.
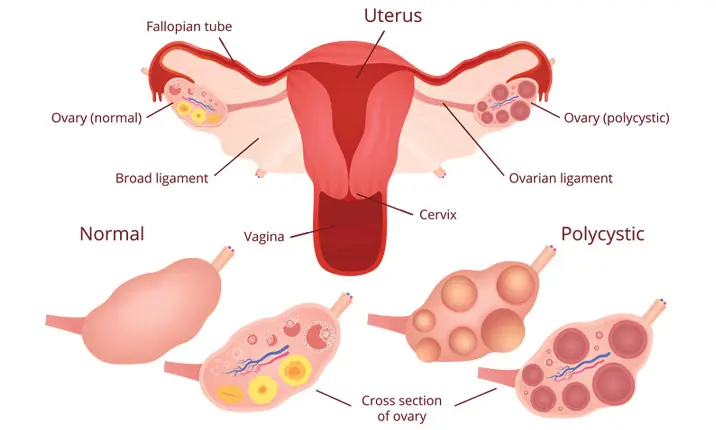
What are ovarian cysts?
Your ovaries are responsible for producing the hormones that regulate your reproductive system.
They also release your egg that's central to your ovulation cycle. It's also during this monthly ovulation cycle that a cyst – a fluid-filled sac – on one or both ovaries, may form.
Cysts can be benign or malignant.
- Benign cysts include endometriotic chocolate cysts and dermoid cysts.
- Malignant tumours include epithelial ovarian cancers, or germ cell tumours.
Cysts usually occur without symptoms, when one of the follicles responsible for releasing the egg fails to open. They usually resolve on their own within a few months without you noticing.
Because most ovarian cysts occur during the ovulation cycle, they are less common in women who have gone through menopause.
What are the symptoms of ovarian cysts?
Symptoms and complications arise if a cyst grows abnormally large or ruptures.
Women who suffer from polycystic ovary syndrome often see numerous small cysts developing on their ovaries. This is a common cause of infertility.
What is the difference between an ovarian cyst and fibroids?
The key difference between an ovarian cyst and fibroids, is that cysts can sometimes go away on their own without ever causing symptoms.
Should you experience bloating, abdominal pressure, pelvic pain, pain during intercourse, consult your gynaecologist for an accurate diagnosis. If the pain is sudden and sharp, especially if accompanied by vomiting and fever, seek urgent medical attention at the [Urgent Care Centre (UCC)](/urgent-care-centre/overview “Urgent Care Centre”).
How are ovarian cysts treated?
If you have been diagnosed with an ovarian cyst, your gynaecologist may take a wait-and-watch approach to see if it resolves on its own.
Pelvic ultrasound
If your doctor has advised a wait-and-watch approach, your condition will be monitored using periodic pelvic ultrasounds.
A pelvic ultrasound uses high-frequency sound waves to create an image of your uterus and ovaries. This will help your doctor to confirm the presence of the cyst, its location and its properties.
Cancer tumour marker blood test
Your doctor may also recommend a tumour marker blood test, known as CA125, to be performed to assess the risk of malignancy. The test detects elevated levels of cancer antigen 125, which is common in women with ovarian cancer.
Birth control pills (oral contraception)
If you have recurrent ovarian cysts, you may be prescribed birth control pills. This helps to prevent the formulation of future cysts during ovulation.
While this will not shrink an existing cyst, birth control pills can reduce your risk for ovarian cancer.
Minimally invasive laparoscopic surgery
If the cyst is a cause for concern, your gynaecologist may make use of a minimally invasive procedure called laparoscopic surgery to investigate the condition.
The procedure makes use of a tiny camera that is introduced through tiny key-hole sized incisions in the abdomen.
Cystectomy
During laparoscopic surgery, your gynaecologist may also remove the cyst. This is known as a cystectomy, which removes the cyst while leaving the ovary intact.
Oophorectomy
For some women, an oophorectomy (removal of one or both ovaries) may be necessary if the ovary or ovaries cannot be saved.
There are several variations of the procedure that may be performed:
- Unilateral oophorectomy removes one ovary
- Bilateral oophorectomy removes both ovaries
- Salpingo-oophorectomy removes one ovary and the fallopian tube which guide eggs from the ovary to the uterus
- Bilateral salpingo-oophorectomy removes both ovaries and fallopian tubes
- Hysterectomy with salpingo-oophorectomy removes the uterus (hysterectomy), and one or both tubes/ovaries.
If both ovaries are removed, you will no longer be able to produce eggs or ova and menopause will begin immediately.
Early diagnosis of ovarian cysts and fibroids
Early diagnosis and treatment are key to successful treatment of both cysts and fibroids.
Cysts and fibroids may initially develop without symptoms. However, when they increase in size or number, symptoms are more likely to appear and it is best to seek medical advice sooner rather than later as earlier diagnosis often improves treatment outcomes.
Make an appointment to see your gynaecologist should you notice any worrying symptoms.