Understanding Pelvic Floor Disorders
Pelvic floor disorders encompass all conditions affecting the normal functioning of the pelvic organs, namely the urinary bladder, the uterus and vagina for the ladies, the prostate for the gents, and anorectum.
These conditions can lead to dysfunction in the pelvic organs, causing issues such as urinary incontinence, vaginal prolapse or bowel incontinence. Often, pelvic floor disorders arise from the laxity of pelvic ligaments and weakness in the pelvic floor muscles. These problems lead to excessive descent of the pelvic organs, and hence, their dysfunction. However, pelvic floor disorders do not encompass cancers of these pelvic organs.
Problems in the pelvic floor can be classified into 3 compartments; anterior (for the bladder), middle (for the uterus/vagina) and posterior (anorectum). A patient may suffer from dysfunction of one or more of the 3 compartments concurrently.
What are some of the common symptoms?
The symptoms experienced depend on which compartment of the pelvic floor and organs are affected.
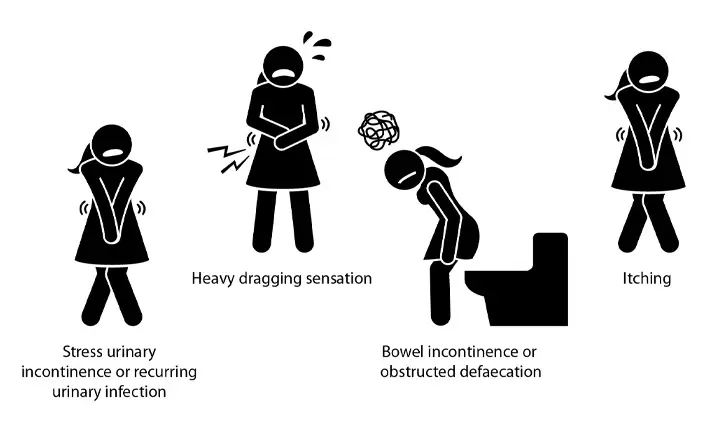
Common symptoms of urinary bladder dysfunction include the leakage of urine when one coughs or sneezes (stress urinary incontinence) or recurrent urinary infection.
Women with vaginal prolapse often feel a heavy dragging sensation in the pelvis and may notice a prolapse of the uterus out of the vagina.
If the problem is in the posterior compartment, the patient may notice the leakage of bowel contents (bowel incontinence) or even difficulty passing motion (obstructed defaecation).
Another common symptom of pelvic floor disorders is itching around the opening of the urethra (urine passage opening), vagina or anus.
What are the different types of pelvic floor disorders?
As pelvic floor disorders affect 3 different pelvic organs, the patient may experience problems with one or more of these organs. Should a patient need treatment for multi-organ problems, there may be a need to have 2 or more specialists involved to coordinate the treatment.
Anterior compartment problems are related to urinary problems and may be treated by urologist or gynaecologists specialising in urinary disorders (urogynaecologists).
Middle compartment problems (such as uterine prolapse) often present at the same time as urinary problems and are best treated by a urogynaecologist.
When there is a problem with bowel control, it is best to seek treatment from a colorectal surgeon specialising in functional defaecatory disorders.
What are the treatments available for a pelvic floor disorder?
Treatments vary from medication to rehabilitative physiotherapy focused on the pelvic floor, and even surgery. For effective control of the pelvic floor disorder, a combination of the various options is commonly utilised.
With a focus on the treatment of pelvic floor disorders that affect defaecation, treatment first involves a detailed understanding of a patient's daily diet, lifestyle and bowel habits.
Patients will be taught how to make dietary and lifestyle adjustments, and undergo anorectal biofeedback. This is a form of pelvic floor rehabilitation aimed at improving a person's control over their abnormal bowel habits.
Patients with bowel incontinence are taught to improve the pelvic floor and anal muscle strength while patients with obstructed defaecation are taught coordination methods to relax the pelvic floor muscles when passing motion. Medication is used to normalise a patient's stool content to prevent diarrhoea or constipation.
Following a period of assessment, surgery may be required if there is no improvement to the condition. Surgical options may involve repairing of the pelvic floor and anal sphincter muscle, tightening of pelvic ligaments or augmenting of the pelvic ligaments with a plastic mesh. Other options include injection therapy to strengthen the anal sphincters for bowel incontinence, implantation of artificial bowel sphincters or implanting an electrode with pacemaker (sacral neuromodulation) to enhance anorectal control.
What do patients have to take care of before and after treatment?
Treatment for pelvic floor disorders will take time, although the options are safe with minimal risk of complications.
Not every patient requires surgery and the aim of every treatment plan is to allow a patient to regain control over the function of their pelvic organs. There is no quick-fix procedure to treat pelvic floor disorders and as a person grows older, the problem may recur as the pelvic floor muscle weaken – but this can be treated with very good results.
Most treatments can be performed easily, either within the day or with no more than a short hospital stay. A patient can usually return to his or her daily routine within a week post-surgery.
Can pelvic disorder lead to more serious illnesses?
Thankfully, pelvic floor disorders are not associated with cancer. However, a cancer can co-exist with a pelvic floor disorder. For example, rectal cancer can be present with bowel incontinence or uterine cancer with uterine prolapse. Doctors usually exclude the possibility of colorectal cancer prior to the treatment of bowel incontinence or obstructed defaecation.
While pelvic floor disorders are not associated with pelvic organ cancers, they may cause pain, infection and bleeding if left untreated. Treatment at an earlier stage will provide better results as treatment halts the progression of the pelvic floor weakness.