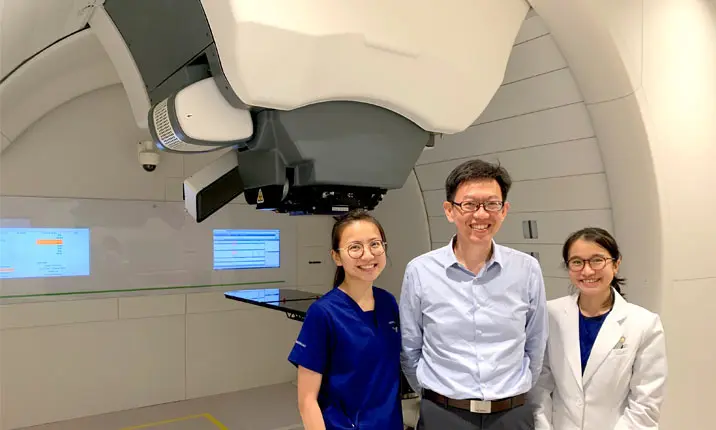
Meet Dr Ivan Tham, radiation oncologist at Mount Elizabeth Hospitals and Gleneagles Hospital, who has been practising radiation oncology in Singapore for nearly 20 years.
He was formerly the head of the radiation oncology departments and a senior consultant at the National University Hospital and Tan Tock Seng Hospital.
He is now a member of the core team at the Mount Elizabeth Proton Therapy Centre at Mount Elizabeth Novena Hospital. At the centre, our patients can access a special type of radiation therapy, called proton therapy.
Get to know Dr Tham and learn more about what he does.
Can you walk us through a typical day in your life as a radiation oncologist?
My practise is across 4 hospital sites – the radiation oncology departments at Mount Elizabeth Novena, Mount Elizabeth Orchard, and Gleneagles Hospital, and the proton therapy centre at Mount Elizabeth Novena.
As such, I start my day with a strong coffee as I check my schedule and organise my priorities. I spend a large part of my day seeing new patients, reviewing patients on treatment, as well as following up on my patients after completion of their cancer treatment.
As radiation oncologists, we can not only prescribe medicine like other doctors, but we can also prescribe radiation. Unfortunately, prescribing radiation is not just about scribbling on a prescription pad and sending it off to the pharmacy.
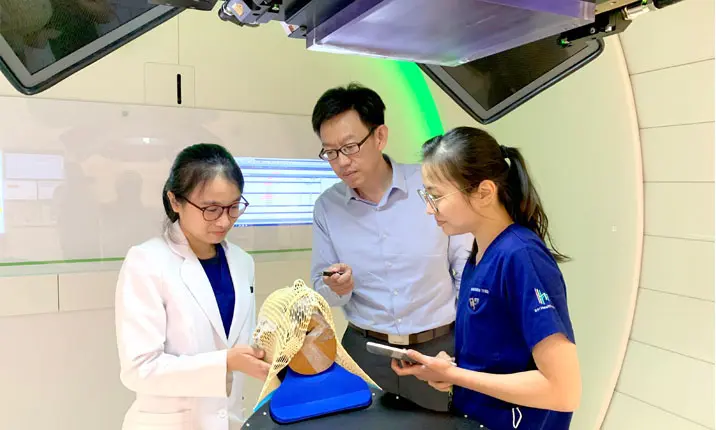
It is a multi-step process where we mark out the tumour targets and normal structures, and work with our colleagues (dosimetrists or medical physicists) to optimise the best way to direct the radiation to a particular patient’s tumour.
This can take up quite a bit of time, especially for complex cases, such as with nasopharyngeal cancer, where there are multiple tumour targets and many normal structures in the head and neck region to avoid. This planning process is similar whether we use X-rays or protons for treatment.
What is proton therapy, and how is it different from standard radiation therapy?
In standard radiation therapy, we generally use X-rays to target the tumour in the body. Typically, we use multiple angles so that the radiation dose will be concentrated in the tumour. This works very well in many situations. However, the surrounding areas will receive some radiation – what we call the “low dose splash”.
In contrast, with proton therapy, we are able to programme the proton beams to stop at a certain depth in the body, just deep enough to treat the tumour without overshooting. This reduces the “low dose splash” area, which helps to minimise side effects.
How does your team of specialists treat patients using proton beam therapy?
A Japanese author once said, “Individually, we are one drop. Together, we are an ocean.” I think this aptly describes any medical team working together to deliver complex care.
Our medical team comprises of doctors, radiation therapists, medical physicists, and nurses. At the Mount Elizabeth Proton Therapy Centre, I work with the physicists to design a suitable radiation treatment plan. The radiation therapists position the patient accurately in the treatment room and deliver the planned radiation treatment. Nurses help with the general medical care of the patient, for example, children who require sedation during their radiation therapy sessions.
Are there specific cancers that are best treated using proton therapy?
Broadly speaking, young patients, or patients with large or deep tumours will benefit more from proton therapy, compared to other forms of radiation treatment.
Younger patients (below 25 years old) generally can have more long-term radiation side effects compared to adults. These include growth impairment, reduction of IQ (if treating the brain) or even possibly second cancers. By reducing the “low dose splash” area surrounding the treatment area, proton therapy can lower these risks compared to X-ray treatment.
When we have to treat large or deep tumours, we can spare normal organs better using proton therapy. For example, if we treat lung or oesophageal cancer, the radiation dose to the heart and normal lungs can be reduced with proton therapy compared to X-ray treatment.
Patients who require chemotherapy treatment during radiation may also benefit from proton therapy because side effects may be reduced.
On the other hand, patients with very small targets, for example, small brain metastases, will not benefit from proton therapy, and will continue to receive stereotactic radiosurgery or stereotactic body radiation therapy using X-rays or gamma rays.
What inspired you to become a radiation oncologist?
I think cancer is appropriately termed a “dread disease” because it is so challenging to treat. When I was choosing my specialty 20 years ago, I was drawn to the field of oncology because I could see that treatment could make such a big difference in a patient’s life. At the same time, radiation oncology was evolving rapidly with improvements in technology.
20 years later, I’m very happy to be able to work at this state-of-the-art facility, which brings together many technological advances.
What do you enjoy most about your work as a radiation oncologist?
Seeing cancer survivors return to a normal lifestyle after treatment.