Wear and tear in your back
The spine, commonly called the backbone, provides support to our body and allows us to move flexibly. As we age, the spine undergoes degenerative changes due to wear and tear from everyday living.
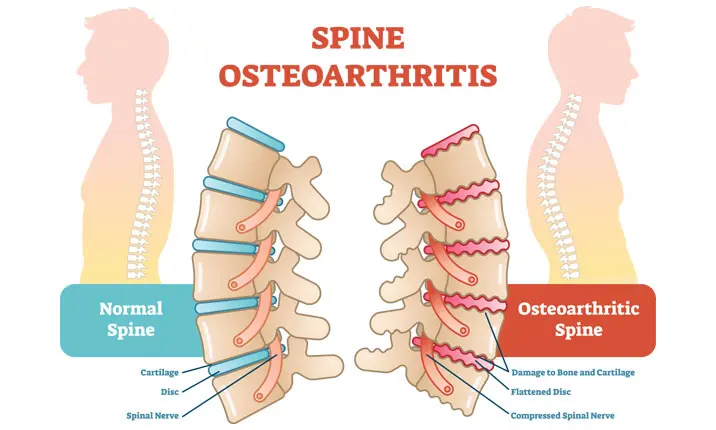
These changes can affect any part of the spine, including the bones, joints, ligaments (strong fibrous bands that stabilise the spine), and discs (soft structures between the bones that act as shock absorbers).
Over the years, this wear and tear of the spine can result in the gradual loss of our spine's normal structure and function.
What are the symptoms of wear and tear of the spine?
Age may just be a number, here's how we can tell that the everyday use of our spine in daily activities is beginning to cause some troublesome symptoms. Many of them can cause inconvenience to our daily activities.
These symptoms include:
- Back pain
- Deformity of the back
- Difficulty in movement
- Loss of sensation in the body
- Muscle weakness
- Problems in urination or defecation
- Sexual dysfunction
What are some possible complications?
With ageing comes wear and tear. As our spine ages along with our bodies, complications such as spinal arthritis or spinal stenosis can develop.
Spinal arthritis
Spinal arthritis is a condition wherein the joints of the spine are inflamed. Although commonly caused by wear and tear, it may also be caused by infections or autoimmune diseases such as rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, reactive arthritis, and enteropathic arthritis.
People with spinal arthritis can experience the following symptoms:
- Back pain and neck pain
- Numbness, pain or tingling in the arms or legs
- Stiffness of the spine
- Swelling of the affected part of the spine
- Weakness and fatigue
The risk of developing spinal arthritis is higher among people who are aged 60 and older, obese, and female. Others at risk include those with a history of back injuries (such as trauma), people with jobs that place recurring strain on the back (such as work which involves heavy lifting), and people with scoliosis.
Spinal stenosis
Spinal stenosis develops when there is narrowing of the spaces within the spine. This condition most commonly affects the neck and lower back portion of the spine.
Spinal stenosis can develop as a consequence of spinal arthritis. If the inflammation in spinal arthritis persists, there can be formation of bony projections in the spine, called bone spurs. These spurs can impinge into the spaces of the spine and cause spinal stenosis.
Wear and tear of the spine can cause the discs to protrude into the spine, or cause the ligaments of the spine to thicken. These conditions also lead to spinal stenosis. Besides natural wear and tear, other possible causes of spinal stenosis are traumatic injuries leading to dislocation or fracture of the bones in the spine, and development of tumours in the spine.
The symptoms of spinal stenosis include:
- Back pain or neck pain
- Numbness, pain or tingling of the extremities
- Problems in balance or walking
- Problems in urination or defecation
- Weakness
The risk of developing spinal stenosis is higher among people aged 50 and older, and those with back injuries caused by trauma, scoliosis, or with genetic conditions that affect bone and muscle development.
How can you prevent spinal complications?
Prevention is always better than cure, especially when it comes to protecting our back. The following strategies can help us take better care of our backs, promote a healthy spine and prevent degenerative complications:
- Do not lift objects that are heavier than 25% of your body weight.
- Do not smoke.
- Eat a healthy diet. Make sure that you have adequate sources of calcium.
- Exercise regularly to maintain a healthy weight and strengthen your back and core muscles.
- Maintain a proper posture.
- Stretch regularly.
How are spinal conditions diagnosed?
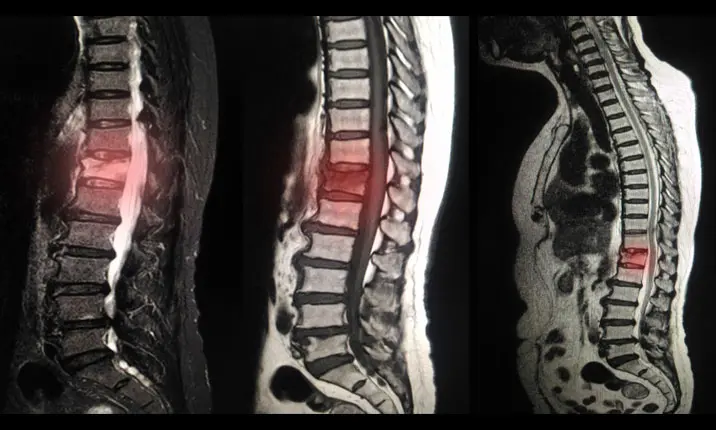
The following tests can also be done to confirm the diagnosis:
- X-ray, CT scan (computerised tomography scan) or MRI (magnetic resonance imaging) of the spine
- Bone scan
- Electromyelogram, a procedure that assesses the health of your muscles and the nerves that control them
How are these complications treated?
Often times, doctors will prescribe pain relievers and physical therapy as the first-line of treatment for these conditions.
However, surgery will be recommended if your symptoms are very severe, such as when pain persists despite medication and physical therapy, or if there are signs of pressure on your spinal nerves.
The type of surgery that is done for spinal arthritis or spinal stenosis is called laminectomy.
Laminectomy, which is also called spinal decompression surgery, is performed by orthopaedic surgeons. It involves the removal of the lamina, which is the back portion of the spine. The aim of the procedure is to create more space in the spinal canal to relieve the pressure on the spinal nerves. In some circumstances, stability of the operated parts of the spine may be improved with the use of screws, rods or bone grafts.
When should you see a doctor for your back pain?
It is best to consult a doctor if you experience any of the following:
- Persistent back pain
- Problems in balance or walking
- Problems in urination or defecation
- Severe back pain
- Weakness, numbness, or tingling in the arms or legs
An orthopaedic specialist will be able to accurately diagnose the cause of your symptoms and suggest suitable treatment options.