Haemorrhoids, or piles, is very common. They are enlarged blood vessels, sometimes described as varicose veins, that occur inside, and around, the anal passage. These are small round lumps that you may feel on your anus, or even notice when they hang outside the anal canal.
What causes piles?
Anyone can get haemorrhoids or piles, but they are more common as you get older. Haemorrhoids form when the naturally occurring blood vessels on the inside of the anal canal become larger and get engorged with blood. This can be caused by regular constipation and straining when trying to pass motion. Piles are also common during pregnancy with the change in hormone levels, and pressure of the baby on the pelvis. Being overweight and having a family history of piles also makes one more susceptible to the condition.
How can you tell if you have piles?
You should see your doctor if you notice lumps around your anus, especially if they cause you pain. Other notable symptoms include the presence of slimy mucus on your underwear, slimy mucus or bright red blood on the toilet paper after passing motion. You may also feel like your bowels haven’t been completely emptied after passing motion.
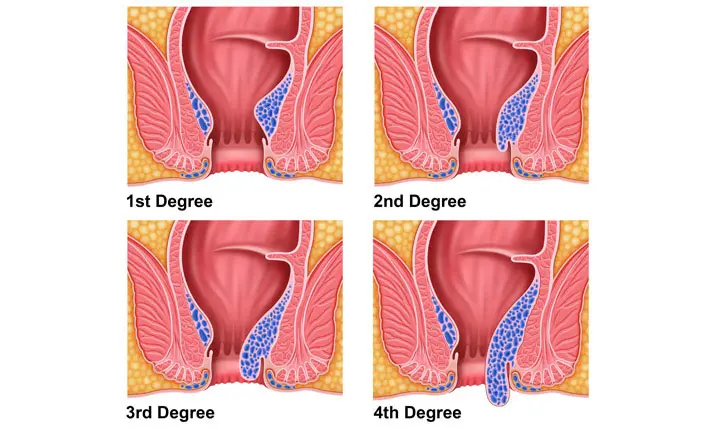
Piles may occur internally or externally. Both conditions may also occur together at the same time. Your symptoms may differ depending on the stage of your condition:
- First degree: Piles are not prolapsed, remaining inside the anus. Light bleeding may still be observed.
- Second degree: Piles may prolapse, or emerge from the anus, with pressure. This may happen with straining during bowel movement, and will spontaneously shrink and retract into the anus after.
- Third degree: Piles emerge during bowel movement, and may not retract on their own. You may feel them hanging from the rectum. Treatment may be required to prevent further pain and infection.
- Fourth degree: Piles remain outside the anus and cannot be pushed back in. They are often large in size and treatment will be required.
What can you do to avoid getting piles?
The best way to avoid getting piles is to prevent constipation, which can be achieved by maintaining a moderate-fibre diet, drinking plenty of water and exercising regularly. Try not to hold off bowel movements for too long, and avoid sitting on the toilet for an extended amount of time to read or use your mobile phone, as this puts extra pressure on the blood vessels in the anus.
How can piles be treated?
Your piles may go away on their own with healthy lifestyle choices that reduce constipation such as maintaining a moderate-fibre diet, drinking plenty of water and exercising regularly.
However, if the piles are causing you pain, talk to your doctor about your treatment options. Your doctor will likely recommend medicated creams or ointments to ease your symptoms. These can be over-the-counter pain and anti-inflammatory medications you can get from the pharmacy. If the inflammation is severe, your doctor will prescribe a corticosteroid cream.
Non-surgical (minor) procedures
If the medications do not work, your doctor may recommend one of the following day procedures, in which you will be awake, but the area will be numbed to avoid discomfort:
- sclerotherapy – a chemical is injected into the haemorrhoid to decrease its size, which will happen over several weeks
- rubber band ligation – a method to cut off the blood supply to the haemorrhoid by tying an elastic band around it, causing it to fall off in up to 10 days
- electrotherapy – a gentle electric current is applied to your piles to shrink them
- infrared coagulation – an infrared light is applied to shrink the piles by cutting off blood supply
Surgical treatment
If your piles improve over time, surgery will not be required. However, if medication and non-invasive procedures don’t work, or if your piles continue bleeding, your specialist may recommend the following surgical procedures:
- Haemorrhoidectomy – complete surgical removal of the piles
- Stapled haemorrhoidopexy – removal of piles via use of a special stapler device. This method, if suitable, is less painful than “conventional” haemorrhoidectomy.
What are the potential complications from surgery?
Surgery should solve your pile problems. But with any surgical procedure, there are risks. These include excessive bleeding or infection. Others include:
- Anal stricture – If the surgical wound heals with a thick scar, this could result in narrowing of the anal passage. Sometimes this may require further surgery to resolve.
- Retention of urine – This is a rare occurrence where there may be some difficulty in passing urine as a result of post-operative discomfort. This may require temporary insertion of a urinary catheter in some patients.
Speak to your doctor about these potential risks, side-effects, and any other concerns you may have regarding the surgical treatment of piles.
When should you visit the UCC?
You should call an ambulance or head straight to the Urgent Care Centre (UCC) if your symptoms change rapidly and you observe the following:
- Bleeding that cannot be stopped
- Severe pain
- The water in the toilet bowl turns red and you see large blood clots
With proper management, you should be able to resolve any flare-up of haemorrhoids as they happen. However, if they are causing you pain or you notice bleeding, seek medical advice from a doctor.