Trigger finger is one of the most common causes of hand pain in adults. The condition can limit your finger's movement and make it difficult to straighten and bend your finger.
Dr Aaron Gan tells us more about trigger finger.
What is trigger finger?
Trigger finger, also known as stenosing tenosynovitis, is a condition where you experience pain and swelling at the base of the finger. Any finger, and more than one finger, can be affected by this condition. When you extend the affected finger from a clenched position, it may jerk, snap or click – much like the trigger of a gun when initiating fire. This is why it is named trigger finger.
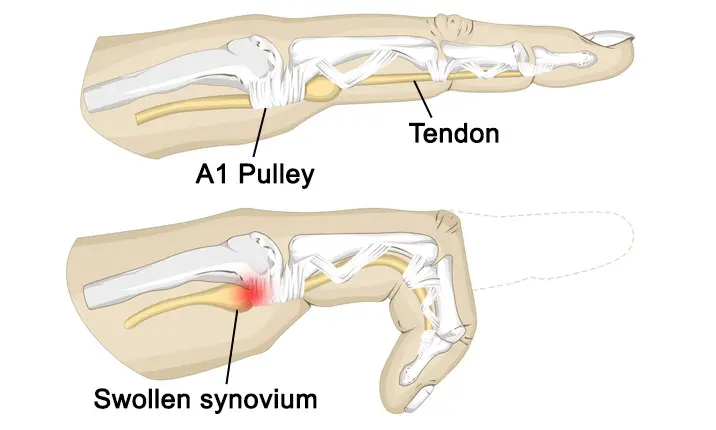
The tissues involved in bending and straightening your fingers in the hands and arms include:
- Tendon – a fibrous connective tissue that connects muscles to bones
- Pulley – the ligaments holding the tendons in place on the bones
What are the causes of trigger finger?
Tendons are surrounded by a sheath of tissue called synovium, a lubricating membrane that surrounds our joints, enabling the tendon to glide easily. A trigger finger occurs when inflammation narrows the space within the sheath surrounding the flexor tendon, which connects the muscles of the forearm to the bones, in the affected finger.
Inflammation is most common at the A1 pulley region, located at the base of each digit at the palm area. It is caused by a swelling of the flexor tendon synovium, which may feel like a nodule, or small lump. As the affected finger is extended, the thickened pulley catches on the nodule as the tendon tries to slide through the sheath. The nodule gets stuck, causing the finger to lock in a bent position. When more force is applied to straighten the finger, the nodule pops through the pulley, causing the triggering phenomenon. In cases where the tendon swelling and sheath tightening are severe, you may not even be able to fully flex the affected finger.
Risk factors of trigger finger
Trigger finger is commonly linked to age, and existing medical conditions such as diabetes mellitus, rheumatoid arthritis, and gout. However, the causes of most cases of trigger finger are unknown. It is believed that the constant or repetitive overuse of the fingers causes accumulated wear-and-tear at the interface between the flexor tendon and the A1 pulley. Over time, this could cause swelling and inflammation of the flexor tendon, and the development of trigger finger.
What are the symptoms of trigger finger?
The symptoms may start out mild before they worsen over time. Triggering of the finger often occurs in the morning, when you grip something or when you straighten your finger.
Symptoms include:
- Finger stiffness, especially in the morning
- A painful clicking or snapping sensation when you bend or straighten a finger
- Soreness or a bump in the palm at the base of the affected finger
- The affected finger catches or locks in a bent position, which suddenly pops straight
- The affected finger is locked in a bent position, which you can't straighten
When should I see a doctor about my trigger finger?
You should seek medical help without delay if your finger joint is hot and inflamed, as these may point to an infection. Delaying treatment when the above symptoms are present will cause you further pain and inconvenience.
How is trigger finger diagnosed?
Your surgeon will first ask for your full medical history before conducting a clinical examination of your hands. The severity of the trigger finger and your condition may be graded by your surgeon as follows:
| Grade I | There is evidence of inflammation at the A1 pulley region of the affected digit, but no demonstrable triggering is noted |
|---|---|
| Grade II | There is evidence of inflammation at the A1 pulley region of the affected digit with demonstrable triggering when the patient is asked to extend the digit from a fully flexed position |
| Grade III A | Same observations as in grade II, but in addition, the patient is unable to fully extend the digit actively as it gets locked in a flexed position, and is achieved only with assistance of the other hand |
| Grade III B | The patient is unable to fully flex the digit due to the severe inflammation at the A1 pulley region |
| Grade IV | There is a fixed flexion deformity at the proximal interphalangeal joint due to longstanding inflammation |
How is trigger finger treated?
1. Medications
This involves taking a course of oral non-steroidal anti-inflammatory medication (NSAIDs) such as ibuprofen, combined with hand therapy, splinting and activity modification. Generally, this is recommended only for patients suffering from trigger finger for the first time or those with grade I or early grade II disease.
2. Splinting
A splint is used to hold your finger or thumb in place and prevent movement. Wearing one overnight may help if your finger usually feels stiffer in the morning. It's more suitable for short-term relief.
3. Therapy
There are several treatment options that can relieve pain and aid in recovery. Depending on the severity of your condition, one or more of these may help.
Rest
Start by avoiding the activities that contribute to trigger finger, such as actions that require repetitive gripping or using tools or equipment that cause vibrations.
Stretching exercises
As trigger finger affects your range of movement, exercises to stretch your finger help to relieve pain and improve flexibility. Aim to spend 15 minutes a day on simple exercises such as palm presses – place a small ball or a similar object in the palm of your hand and squeeze tightly for several seconds before releasing and spreading your fingers wide.
Ice therapy
Applying an ice pack can help to reduce the inflammation and ease the pain. Try it several times a day for no more than 10 minutes at a time.
Physiotherapy
Physiotherapy can help you to regain your finger's strength and range of motion. Speak with your doctor about stretches and exercises that might help, and avoid activities that require repetitive gripping or grasping, or the use of hand-held equipment that causes vibrations.
4. Corticosteroid injections
This involves an injection, directly into the flexor tendon sheath. The injection contains a mixture of a local anaesthetic (numbing) agent and a corticosteroid preparation.
A corticosteroid injection helps to reduce swelling in the tendon, which will help to relieve pain. It's estimated to be effective for 50 – 70% of people, with noticeable results within a few days or several weeks.
This resolves the inflammation at the A1 pulley site and relieves the trigger finger. This effect may or may not be longlasting, and recurrence is always a possibility. Repeated injections should not be attempted. Hand surgeons advocate a maximum of 2 injections to an affected digit, except the little finger, which should not have more than 1 injection.
The belief is that corticosteroids weaken the tendon and can result in atraumatic tendon rupture (tear) if subjected to repeated injections. This treatment is recommended when non-invasive treatment fails to work, and for grade II or III triggers.
5. Surgery
This involves releasing the A1 pulley, pre-annular pulley, and even part of the A2 pulley, if necessary, through a small skin incision made at the base of the digit.
It is rare for trigger finger to recur after surgery. For grade IV trigger finger, the surgeon may perform an additional procedure to release the proximal interphalangeal joint, the hinge joints between the digital bones of the fingers that provide flexion towards the palm, which has become stuck due to longstanding stiffness. A separate incision over the proximal interphalangeal joint is necessary for such a procedure.
What kind of specialist should I see to treat my trigger finger?
It would be best to see a hand surgeon, who is experienced in managing conditions of the fingers, hands and wrist exclusively. Hand surgeons are well-equipped with skills and knowledge to handle all grades of trigger finger. Hand surgery centres also have in-house hand occupational therapists who provide hand therapy and specialty splints, such as a figure-of-eight splint, which are used in the treatment of early grade trigger fingers. Hand surgeons are trained to give accurate intra-thecal flexor sheath injections to maximise the possibility of cure and minimise the chance of recurrence. If surgery is required, hand surgeons perform the most meticulous operation to release the trigger. Skin incisions are made within the natural crease lines to achieve a virtually scar-free result.