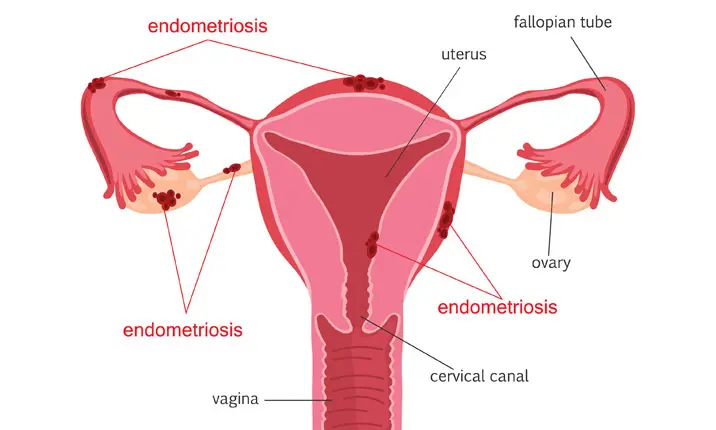
Understanding endometriosis
Endometriosis is a painful condition where the cells from the inner lining of the womb grow outside the uterus and in the surrounding areas such as the ovaries, fallopian tubes and ovarian ligaments. The condition can range from minimal growth to severe, where other organs in the body such as the bladder, ureter and bowels may be affected. This tissue implants itself and releases blood and inflammatory chemicals during menstruation, which is why your periods get very painful if you suffer from endometriosis.
Why is endometriosis a growing concern?
About 10% of females worldwide have endometriosis, but this figure could in fact be much higher as some women go undiagnosed, thinking their periods are normal. The condition is more prevalent now due to better socio-economic status, delayed childbearing and also fewer pregnancies. While the exact cause is not known, it is believed that endometriosis occurs when blood containing cells from the endometrium flows backwards into the pelvic area via the fallopian tubes during menstruation. This backflow carries the cells to other organs like the ovaries, rectum and pelvic ligaments, and causes other problems.
When you may be at risk
You are more likely to develop endometriosis if there is a history of it in your family, if you delay childbirth and have fewer children or if you don't give birth at all. If you have a medical condition that prevents normal menstrual flow, you are also at higher risk. If you have endometriosis and your condition is severe, you may have difficulty conceiving, develop anaemia, have other organs affected and may even be at risk of developing cancer.
If left untreated, endometriosis is likely to worsen. More pelvic organs will be affected, and implants can infiltrate deeper into the nerves, organs and tissues. When the small capillaries and nerves get involved, the pain becomes worse.
Endometriosis can lead to infertility when inflammation causes the fallopian tubes to be blocked. Another complication is endometriosis-related cancers, most commonly ovarian cancer. Your chances of developing ovarian cancer could be 2 – 3 times higher if you have endometriosis.
When to see a doctor
Your period should not interfere with your ability to go about your normal day-to-day activities. If you find your periods debilitating and you are skipping social activities or work and have any of the following symptoms, talk to your doctor for an early diagnosis so that you have more and less-invasive treatment options available.
- Severe pain during menstruation
- Heavy periods
- Cold sweat, nausea or near fainting spells
- Painful intercourse
- Lower back pain
- Bloating and abdominal swelling
- Chronic fatigue
- Infertility
What to expect when you consult your doctor
You will be referred to a gynaecologist, who will assess your symptoms and family history. If endometriosis is suspected, your gynae will secure a definite diagnosis through minor keyhole surgery called a laparoscopy. A thin, pencil-like instrument with a camera will be inserted into your abdomen to view your internal organs and to obtain a biopsy, the removal of a small amount of abnormal tissue. This will be sent to the lab for diagnosis.
Possible treatment options
Medications
Treatment will depend on your age and fertility considerations. If you are young and the condition is not as serious, medications are the first line of treatment. These can include nonsteroidal anti-inflammatory drugs (NSAIDs) and painkillers.
Hormone therapy
Your doctor may prescribe you hormone supplements to help slow down the endometrial tissue growth and prevent new implants. These supplements could be in the form of birth control pills, gonadotropin-releasing hormone (Gn-RH) injections and progestin. The course of treatment needs to continue, or the symptoms could return.
Surgery
If you are planning for a baby or are in severe pain, your doctor may recommend surgery to remove as much endometriosis as possible while preserving the uterus and ovaries. Most endometriosis experts will advise that the first surgery should be as thorough as possible so as not to leave behind tissue that may flare up again. A low-dose progestin-only pill may be a good long-term option to reduce the risk for recurrence. For more serious cases and for women who have completed their family planning, a hysterectomy may be recommended. The ovaries may or may not be removed depending on how extensive the endometriosis is.