Endometriosis is a condition in which tissue that is similar to the lining of your uterus (the endometrium) grows outside of the uterine cavity and spreads to the ovaries, bowel, and tissues lining your pelvis.
The abnormal tissue can cause the area it affects to become inflamed. It can thicken, break down and remain in your pelvis, causing severe pain during your periods, and in some cases even bind pelvic organs together. There is also a risk of infertility, meaning that women who are trying for a child may face difficulty in becoming pregnant.
How do I know if I have endometriosis?
You may experience intense pain even though you have a mild form of the disease, or you may have a serious case and yet feel no pain at all. Your degree of pain should therefore not be used as an indication, stage or absence of the disease.
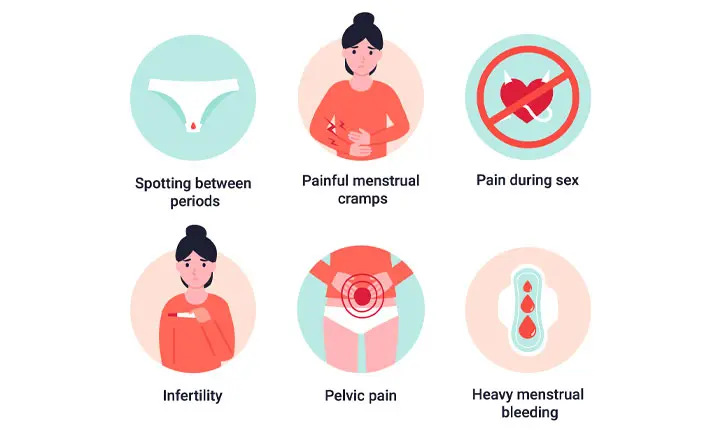
If you have two or more of the following symptoms, do see a gynaecologist for a more accurate diagnosis and treatment plan:
- Pelvic pain (the most common symptom of endometriosis)
- Lower back pain
- Painful periods (but as mentioned above, this alone is not an indication)
- Cramps 1 – 2 weeks around menstruation
- Heavy bleeding during or between periods
- Discomfort during bowel movements
- Problems conceiving
- Pain during sexual intercourse
What causes endometriosis?
There are several theories about the cause of endometriosis. While the exact cause of endometriosis is unknown, here are a few factors that can possibly lead to the condition:
- Retrograde menstruation – This is when menstrual blood flows back through your fallopian tubes into your pelvic cavity instead of leaving your body through the vagina during your period.
- Hormones transform the cells outside the uterus into cells similar to those lining the inside of the uterus.
- Areas of your abdomen convert into endometrial tissue for reasons not yet known. These continue to grow and bleed in response to the hormones of your menstrual cycle.
- Menstrual blood leaks into the pelvic cavity through a surgical scar, such as after a caesarean section.
- Endometrial cells are transported out of the uterus by the lymphatic system, spreading through the body and giving rise to the disease.
- A problem with the immune system that makes the body unable to recognise and hence destroy endometrial cells as they grow.
- Genetics – Endometriosis is more common among women who have a family history of the disease.
- Environmental toxins.
How is endometriosis diagnosed?
Regardless of the cause, it is important that the condition is accurately diagnosed so that appropriate treatment can be received. Your gynaecologist will request for your medical history and perform a physical exam to feel for any tell-tale cysts in your abdomen or scars behind the uterus. You may be sent for an ultrasound which can identify cysts linked to endometriosis.
To get an accurate diagnosis, your gynaecologist may order a laparoscopy (a minimally invasive surgery), which allows the surgeon to view the inside of your pelvis and remove offending tissue at the same time.
I've been diagnosed with endometriosis. What are my treatment options?
While there is no cure for endometriosis, the good news is that, once diagnosed, it can be managed through the reduction of your symptoms and management of potential complications.
Your gynaecologist will recommend more conservative medical treatments to see if your condition responds well before resorting to surgery. As everyone’s response to treatment is unique, there is no way to know how you will respond until you undergo different treatment options. Your gynaecologist will work with you to find the best option for you.
Discuss with your gynaecologist and be open about your mental health as this condition can take an understandable toll, especially in the stage where you are trying to find out which treatment works, dealing with intense pain and handling any fertility issues.
Here are the possible treatments your gynaecologist may take you through:
- Pain medication – Over-the-counter medication can help relieve pain but may not be effective in all cases.
- Hormone therapy – This may help to regulate the hormones promoting tissue growth.
- Hormonal contraception – This can prevent the build-up of tissue. The medroxyprogesterone (Depo-Provera) injection can also be considered but with caution, as there is a risk of decreased bone production, weight gain and depression in some cases.
- Gonadotropin-releasing hormone (GnRH) agonists and antagonists – These work to block the production of oestrogen, which stops menstruation and puts you into an artificial menopause, with all its related side effects.
- Danazol – This is another medication that can stop menstruation but is not always successful at stopping the progress of the disease. Acne and excess facial and body hair are possible side effects.
- Laparoscopy – This diagnostic procedure can also be used to remove tissue growth with lasers without damaging the reproductive organs. It is usually recommended when hormone treatments fail to work or for women who want to get pregnant.
- Total hysterectomy – Your doctor may suggest this surgery as a last resort, to remove your uterus, cervix and often your ovaries. This is recommended if no other treatments have worked and you do not have plans for another child. However, the surgery is not considered a treatment for endometriosis and is considered a last-resort option when nothing else has worked.
What are the complications of endometriosis?
Infertility
About one-third of women with endometriosis face difficulty getting pregnant. Those with a milder form of the condition may be able to conceive and carry a pregnancy to term without assistance, although the condition will have to be monitored throughout pregnancy.
If endometriosis is diagnosed early, your doctor may discuss the possibility of trying for children earlier rather than later as fertility risks grow with the disease.
When you are ready to try for a baby, your gynaecologist will recommend surgery to remove the endometriotic cysts. If this doesn’t work in your case, undergoing fertility treatment may help.
Chronic pain
Managing chronic pain is a further complication of endometriosis. Work with your doctor to manage this as it can be debilitating and affect your daily routines.
Depression
Unsuccessful management of the pain or growing fertility concerns can cause depression and anxiety. Do be open with your gynaecologist about how you are feeling.
Not receiving treatment
If you have endometriosis and decide not to receive treatment, your condition can grow more severe, and you may develop chocolate cysts otherwise known as ovarian endometriotic cysts. These are cysts containing old blood within the ovaries. In some cases, chocolate cysts can stop the ovaries from working and cause infertility.
Seek an early diagnosis
If you suspect you may have endometriosis, book an appointment with your gynaecologist to receive a diagnosis. Even if your symptoms appear to be manageable now, the condition can worsen over time and lead to more difficulties in managing symptoms or complications such as infertility.