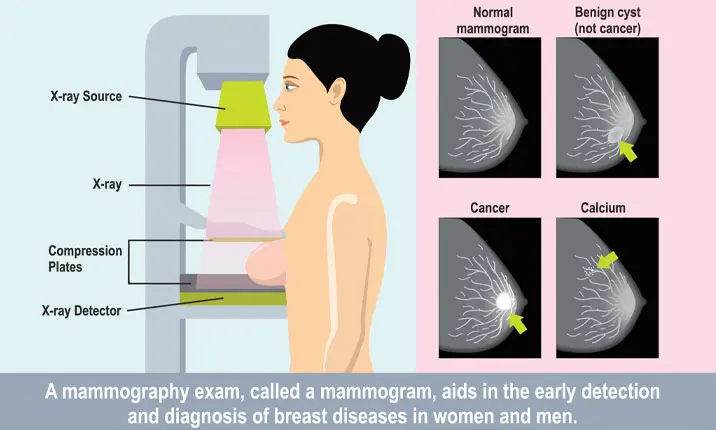
What is a mammogram?
A mammogram is an x-ray picture of the breast. It is a useful tool to look for early signs of breast cancer. Scheduling mammograms regularly is the best way to find breast cancer early, sometimes up to 3 years before it can be felt.
If you are a woman aged 40 and above, schedule a mammogram if you have not had one in the past year or two.
How is a mammogram done?
Shortly before your mammogram, you will be asked to undress from the waist up. You will stand in front of a special x-ray machine for the mammogram.
A technician will position your breast on a plastic plate. There will be a second plate that will firmly press your breast from above.
The plates will compress the breast and hold it still while the x-ray is being taken from several angles. This is because the breast tissue needs to be spread out to detect any lumps or abnormalities in the breast. You will feel some pressure and discomfort.
The steps are then repeated to obtain x-ray images of the other breast.
The x-ray images will be evaluated by a radiologist and you will receive your results at a later date.
Are mammograms painful?
Most women find a mammogram a bit uncomfortable, while some find it painful. The good news is that the test itself only takes a few moments and the discomfort is over soon enough.
What you feel during a mammogram depends on several factors, such as the skill of the technician, the size of your breast, and how much they need to be pressed. Your breasts may also be more sensitive if you are about to get or are having your period.
When to schedule a mammogram?
Take your menstrual cycle into account when you are thinking of having your mammogram. The week after your period is usually the most ideal time to schedule a mammogram.
At what age should you get a mammogram?
Women between the ages of 40 and 44 may start annual breast cancer screening with mammograms if they wish to do so.
Women between the ages of 45 and 54 should get mammograms every year.
Women aged 55 and older may opt to have mammograms every 2 years or can continue with annual screening.
If you have a family history of breast cancer, your doctor may recommend more frequent mammograms for early breast cancer detection. Talk to your doctor about your breast cancer risk to determine the right screening plan for you.
How to prepare for a mammogram?
Remember:
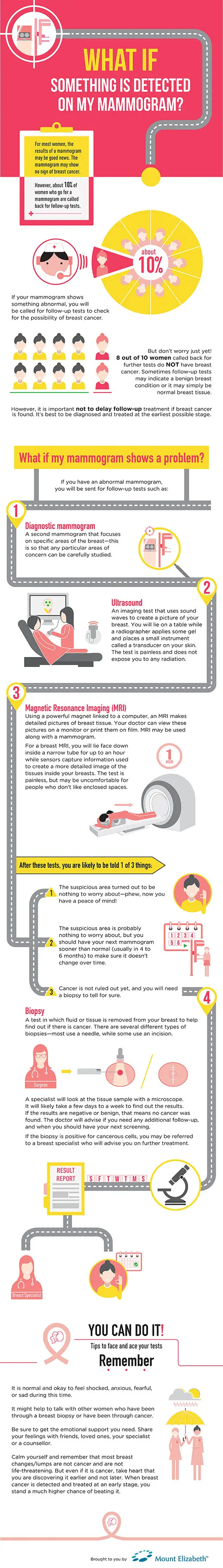
- It is normal and okay to feel shocked, anxious, fearful, or sad during this time.
- It might help to talk with other women who have been through a breast biopsy or have been through cancer.
- Be sure to get the emotional support you need. Share your feelings with friends, loved ones, your specialist or a counsellor.
- Calm yourself and remember that most breast changes/lumps are not cancer and are not life-threatening. But even if it is cancer, take heart that you are discovering it earlier and not later. When breast cancer is detected and treated at an early stage, chances are that you can beat the cancer.
Mammogram results
For most women, the results of a mammogram may be good news. The mammogram may show no sign of breast cancer.
However, about 10% of women who go for a mammogram are called back for follow-up tests.
If your mammogram shows something abnormal, you will need follow-up tests to check whether or not the finding is breast cancer.
But don't worry just yet! 8 out of 10 women called back for further tests do not have breast cancer. Sometimes follow-up tests show a benign breast condition or normal breast tissue.
However, it's important not to delay follow-up. If breast cancer is found, it's best to be diagnosed and treated at the earliest possible stage.
What if I have abnormal mammogram results?
If you have an abnormal mammogram, the follow-up tests you will have depend on the recommendations of the radiologist.
You are likely to have a:
1. Diagnostic mammogram
A second mammogram that focuses on specific areas of the breast – this is so that any particular areas of concern can be carefully studied.
2. Ultrasound
An imaging test that uses sound waves to create a picture of your breast. You will lie on a table while a radiographer applies some gel and places a small instrument called a transducer on your skin. The test is painless and does not expose you to any radiation.
In addition, you may also have an:
3. Magnetic resonance imaging (MRI)
Using a powerful magnet linked to a computer, an MRI makes detailed pictures of breast tissue. Your doctor can view these pictures on a monitor or print them on film. MRI may be used along with a mammogram.
For a breast MRI, you will lie face down inside a narrow tube for up to an hour while sensors capture information used to create a more detailed image of the tissues inside your breasts. The test is painless, but can be uncomfortable for people who don't like enclosed spaces.
After these tests, you are likely to be told 1 of 3 things:
- The suspicious area turned out to be nothing to worry about – phew, now you have peace of mind!
- The area is probably nothing to worry about, but you should have your next mammogram sooner than normal (usually in 4 – 6 months) to make sure it doesn't change over time.
- Cancer is not ruled out yet, and you will need a biopsy to tell for sure.
4. Biopsy
A test in which fluid or tissue is removed from your breast to help find out if there is cancer. Your doctor may refer you to a surgeon or to a doctor who is an expert in breast disease for a biopsy.
There are several different types of biopsies – most use a needle, but some use an incision. The type you have depends on things like how suspicious the tumour looks, how big it is, where it is in the breast, how many tumours there are, other medical problems you might have, and your personal preferences.
A specialist will look at the tissue sample with a microscope. It will likely take a few days to a week for you to find out the results.
If the results are negative or benign, that means no cancer was found. Ask the doctor whether you need any additional follow-up, and when you should have your next screening mammogram.
If the biopsy shows that you do have cancer, your doctor may refer you to a breast specialist.