Peritoneal dialysis (PD) offers a flexible, home-based alternative to haemodialysis (HD), giving you control over your treatment. In this article, we break down everything you need to know about PD – how it works, the different types, and what to expect in terms of time and lifestyle.
What is peritoneal dialysis (PD)?
Peritoneal dialysis (PD) is a form of treatment for individuals with end-stage kidney disease, otherwise known as kidney failure.
It offers an alternative to haemodialysis (HD), allowing patients to manage their dialysis from the comfort of their own home. This treatment uses the peritoneum (a membrane that lines your abdomen) to filter waste and excess fluid from the body.
There are 2 main types of peritoneal dialysis:
- Manual exchanges: Continuous ambulatory peritoneal dialysis (CAPD)
- Machine-based: Cycler-based peritoneal dialysis, also known as automated peritoneal dialysis (APD)
What is continuous ambulatory peritoneal dialysis (CAPD)?
Continuous ambulatory peritoneal dialysis (CAPD) is a manual form of PD that does not require a machine. It allows you to carry on with your daily activities while undergoing treatment.
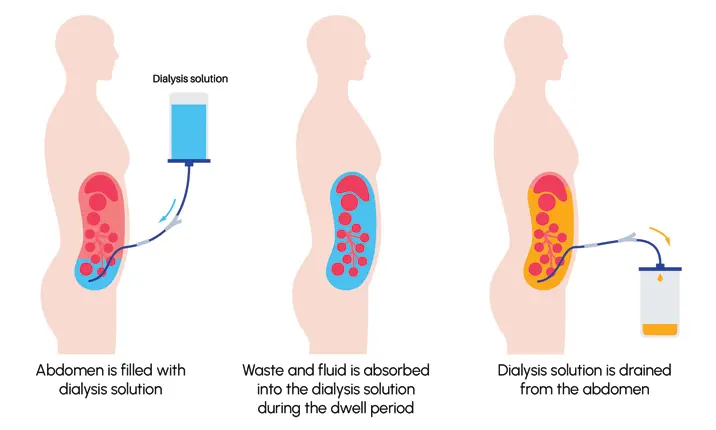
During CAPD, you fill your abdomen with dialysis solution 3 – 4 times a day. The solution remains in the abdomen for a few hours (this is called the "dwell time"), absorbing waste and fluid from your blood. After this period, the fluid is drained and replaced with fresh solution.
Each exchange of the dialysis solution takes about 20 – 30 minutes, and the fluid typically remains in your abdomen for 4 – 6 hours. Since you do not need to be hooked up to a machine, CAPD offers more flexibility, and many patients prefer it because it allows them to move freely. It is similar to taking medications 3 – 4 times a day but requiring about 20 – 30 minutes each time.
Individuals who are working often do an exchange at home during breakfast and bring a bag to work for an exchange during lunch. They continue with an exchange at dinnertime when they return home from work, and a final exchange before they sleep. This minimises the disruption to their work schedule, without a need to rush to a haemodialysis centre. As CAPD allows continuous kidney failure treatment, your doctor has a lot more liberty and flexibility to allow you to stop treatment for 1 – 2 exchanges or even 1 day to accommodate special social circumstances.
What is cycler-based peritoneal dialysis?
Cycler-based peritoneal dialysis, also known as automated peritoneal dialysis (APD), uses a machine called a cycler to perform the dialysis exchanges while you sleep.
The cycler automatically fills and drains the dialysis solution from your abdomen during the night, typically over a period of 8 – 10 hours. In the morning, depending on your medical condition, the doctor may prescribe for the machine to keep your abdomen dry or to fill a certain volume , and you can go about your day without needing to perform further exchanges until the following night.
APD offers convenience, as the treatment is done overnight, which may be preferable for patients who want their days free from dialysis. However, APD requires you to stay connected to the machine for several hours during the night and may disturb light sleepers.
How does peritoneal dialysis (PD) work?
You will typically undergo peritoneal dialysis at home daily.
Before the procedure:
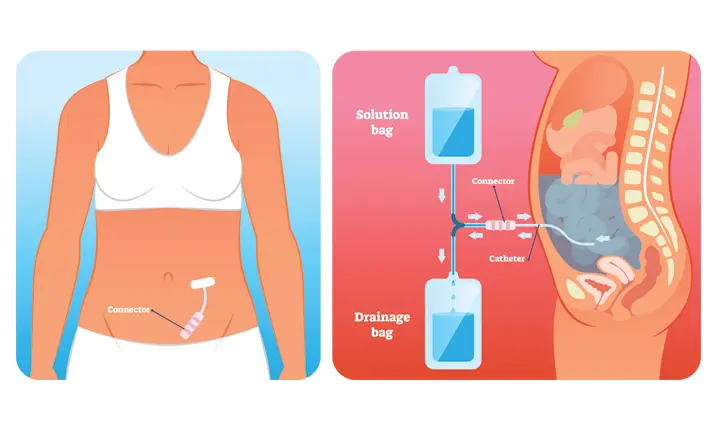
- A catheter is surgically inserted into your abdomen near the belly button. This catheter acts as the conduit for the dialysis solution to flow in and out.
- The catheter insertion is usually done under general anesthesia.
- You will need to wait for about 2 weeks for the catheter site to heal before beginning dialysis.
- Your doctor will arrange for a nurse to train you or your caregiver how to perform the exchanges at home. The training typically requires about 3 days, to ensure that you or your caregiver can perform the exchanges competently and safely.
During the procedure:
- You will fill your abdomen with the dialysis solution. The peritoneum acts as the filter, allowing waste products and excess fluid to move into the solution.
- After the prescribed dwell period (“dwell time”), you will drain the solution and replace it with fresh fluid. This is known as an exchange.
- If you are on APD, the machine will handle the exchanges during the night while you sleep.
Care and recovery after PD:
- You will need to take your medications as prescribed by your doctor and follow a healthy diet, including foods low in sodium and phosphorus.
- You should avoid soaking in baths, hot tubs, or swimming in non-chlorinated bodies of water to reduce the risk of infection.
How long does peritoneal dialysis take?
The duration of peritoneal dialysis depends on the type of dialysis you are using:
CAPD: You will perform 3 – 4 exchanges daily, with each exchange lasting around 20 – 30 minutes. The solution remains in your abdomen for a dwell time of 4 – 6 hours.
APD: You will remain connected to the cycler machine for 8 – 10 hours overnight, allowing the machine to automatically perform multiple exchanges while you sleep.
How long can you live on peritoneal dialysis (PD)?
Many patients can live on peritoneal dialysis for many years.
While there is no definitive lifespan for someone on dialysis, the duration of treatment depends on several factors such as age, overall health, and how well you follow your treatment plan. Some patients may remain on dialysis for 5 – 10 years or longer, while others may eventually receive a kidney transplant, which could eliminate the need for dialysis.
What are the benefits of peritoneal dialysis (PD)?
- Independence: PD can be done at home, offering flexibility and allowing you to maintain an active lifestyle.
- Fewer dietary restrictions: Compared to haemodialysis, PD typically involves fewer dietary and fluid intake restrictions.
- Avoiding hospital visits: Since PD can be performed at home, you avoid frequent hospital visits required for haemodialysis.
- Continuous treatment: PD provides continuous removal of waste and fluid, which may result in fewer fluctuations in symptoms, such as fatigue or low blood pressure, compared to haemodialysis.
- Better infection control: PD does not require the need to access your blood and share machines, hence, there is almost no risk for blood-borne infections like hepatitis B, hepatitis C or HIV. During a pandemic, there is also no exposure to other patients in a haemodialysis centre as the dialysis is done in the safety and comfort of your home.
What are the risks of peritoneal dialysis (PD)?
While PD offers many advantages, there are some risks and complications to be aware of:
- Hernias: The constant presence of fluid in the abdomen can weaken abdominal muscles, increasing the risk of hernias.
- Infection: Infection can occur around the catheter insertion site or inside the peritoneum (peritonitis).
- High blood sugar: The dialysis solution contains sugar (dextrose), which can be absorbed into the bloodstream, potentially leading to high blood sugar levels.
Who should not undergo peritoneal dialysis (PD)?
Peritoneal dialysis may not be suitable for everyone. It may not be recommended if you:
- Have extensive surgical scars in your abdomen.
- Have a hernia, which indicates weakened abdominal muscles. However, once the hernia is repaired, you may be able to start on PD after your doctor’s assessment.
- Have limited dexterity or ability to care for yourself.
- Suffer from inflammatory bowel disease. In such cases, your doctor may recommend haemodialysis or a kidney transplant instead.
Peritoneal dialysis (PD) vs haemodialysis (HD): what's the difference?
The key difference between PD and HD is how and where the treatments are done.
PD uses the lining of your abdomen (the peritoneum) to filter waste and can be performed at home, either manually during the day (CAPD) or with a machine at night (APD).
HD, on the other hand, filters your blood using a machine, and it usually takes place at a hospital or clinic 3 times a week. The patient is usually connected to a machine for about 4 hours.
Survival rate for PD vs HD
Studies have shown that PD has a survival advantage in the first 2 – 3 years of treatment over HD, thereafter, the survival are similar. Therefore, it is better to start with PD first should you require dialysis. In addition, patients who are being planned for a kidney transplant, have better outcomes after the transplant if they were on PD compared to HD. However, the decision on which type of dialysis is best for you should not be based solely on survival rates, but also on how each treatment impacts your quality of life.
According to a 2022 article published by Annals, the official journal of the Academy of Medicine, Singapore, research has found that patients on PD often report a better quality of life than those on HD, likely because PD can be done at home and offers more flexibility.
Ultimately, choosing between PD and HD should depend on several factors, including your daily routine, personal preferences, and specific medical needs.
PD may offer more flexibility for those who prefer the independence of home treatment, while HD might be better suited for individuals who are more comfortable receiving treatment in a clinical setting. Additionally, your overall health, ability to manage home-based care, and any underlying conditions should be taken into consideration.
Your healthcare team plays a crucial role in helping you make an informed decision. They will assess your medical condition, discuss the pros and cons of each option, and tailor their recommendations to your individual circumstances. Speak to our doctors to find the treatment approach that best fits your lifestyle while ensuring your health needs are met.