Singapore has the fastest ageing population in Asia, and life expectancy among women has gone up to 85 years in 2017. As health issues tend to arise with age, it's important for women to be well-prepared for any eventuality.
Here's what you should know about common health problems faced by women over 40.
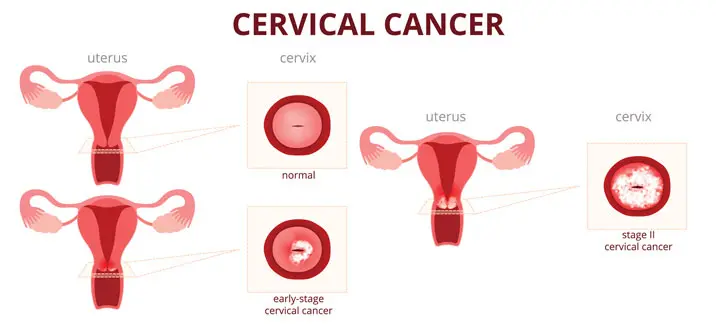
Cervical cancer
Cervical cancer is a type of cancer that forms in the cervix, the lower part of the womb or uterus that connects to the vagina.
Cervical cancer is the second most common cancer among women worldwide and the eleventh most common cancer among women in Singapore. In women aged 15 – 44, it is the fifth most common cancer.
While improvements in screening and early intervention have helped to create a downward trend since the 1970s, the disease may once more be on the rise. Based on current estimates, approximately 309 women in Singapore are diagnosed with cervical cancer every year, resulting in 172 deaths.
What are the causes of cervical cancer?
The human papillomavirus (HPV) causes cancer of the cervix. There are more than 100 types of HPV that can infect humans, but HPV types 16 and 18 cause 70% of cervical cancer cases.
What are the symptoms of cervical cancer?
Symptoms of cervical cancer usually appear only in later stages of the disease. This underscores the importance of screening, so that it can be detected and treated early.
Symptoms of cervical cancer may include:
- Pain in the lower abdomen
- Pain during sexual intercourse
- Vaginal bleeding between periods or after menopause
- Vaginal discharge that is watery, bloody or foul-smelling
Early detection of cervical cancer
Cancer of the cervix is one of the most common female cancers, so sexually active women are advised to go for regular Pap smears or HPV tests.
Pap smear and HPV tests
The Pap smear tests for presence of precancerous or cancerous cells on the cervix, or the opening of the womb.
During a Pap smear, you will lie on an inclined examination table. You will have to spread your legs, with your feet resting in stirrups for support.
A device known as a speculum will be gently inserted into your vagina to keep the vagina walls open, allowing your doctor to use a brush and/or spatula to collect a tissue sample from the cervix. The sample is then sent to a lab to check for abnormalities.
It is normal to feel some pressure and discomfort during the tissue collection process, which subsides after a short time. Some women may temporarily experience mild cramps and light spotting, which should pass within the same day.
The Singapore Cancer Society Women aged 25 – 29 years who are sexually active should aim to get a Pap smear once every 3 years. For women aged 30 years and above, the Singapore Cancer Society recommends HPV tests, which employs the same technique for collecting tissue samples, which are analysed to look for the specific types of HPV that are known to cause cervical cancer.
Ultrasound
Your doctor may also recommend an ultrasound scan of the pelvis to detect growths such as ovarian cysts and fibroids.
A pelvic ultrasound is a non-invasive imaging test that allows doctors to view internal organs and structures such as the uterus, cervix, vagina, ovaries and fallopian tubes.
You will lie down on the examination table, and the doctor will apply ultrasound gel over the area to be scanned. A device known as a transducer, which emits high-frequency waves, will be used to firmly glide over the relevant areas, creating an image of the internal structures including any abnormalities.
Survival rate of cervical cancer
Recovery and survival rates are better when cervical cancer is detected early. In fact, the 5-year survival rate for early stage cervical cancer (stage 0 and stage 1A) is about 93%.
Human Papillomavirus (HPV) vaccination
Today, vaccination against HPV provides good protection against HPV types 16 and 18, which account for 70% of all cervical cancer cases. With minimal risks and complications, HPV vaccination is advocated for prevention of cervical cancer and recommended for girls and women prior to their first sexual encounter. However, women who are already sexually active may still be vaccinated and they should discuss HPV vaccination with their doctor.
In Singapore, the HPV vaccination can be administered to women from 9 – 26 years old, depending on the vaccine that is being administered.
Urinary incontinence and pelvic organ prolapse
Urinary incontinence (leakage of urine) and pelvic organ prolapse (dropping of the womb, bladder or bowel through the vagina) are common urogynaecological problems. In fact, as many as 50% of women may suffer these conditions, yet few are seeking help. These issues can affect not only a woman's quality of life and sexual health but also her work life.
Stress urinary incontinence (SUI)
Stress urinary incontinence (SUI) is the uncontrollable leakage of urine on exertion. Women may leak urine during actions such as running, jumping, sneezing, laughing and coughing. Causes include childbirth, menopause, obesity, chronic lifting of heavy loads, chronic cough, and constipation.
Causes of stress urinary incontinence (SUI)
Causes of SUI include:
- Childbirth
- Menopause
- Obesity
- Chronic lifting of heavy loads
- Chronic cough
- Constipation
A national survey on 3,500 females in Singapore by Dr Chong revealed that 13.5% of them suffered from SUI. In fact, 35.6% of women – that's more than 1 in 3 – aged above 50 may suffer from the condition. Many women did not seek treatment for SUI because:
- They were too embarrassed to talk about it, even with close friends or relatives
- They did not know it is a problem
- They did not know it can be treated and did not know where to seek treatment
Prevention of urinary incontinence
Many women accept urinary incontinence as part and parcel of growing old. It is estimated that only less than 30% of the female sufferers worldwide have sought treatment, even though SUI and pelvic organ prolapse can be prevented. At Gleneagles Hospital, for instance, there is a screening clinic to detect these problems early, and a prevention clinic that teaches patients prevention techniques.
Treatment of stress urinary incontinence
To treat SUI, your doctor may recommend pelvic floor exercises, medication or surgery.
Pelvic floor exercises
Mild SUI can be treated with pelvic floor exercises. If these do not work, or if the SUI is moderate or severe, surgery is usually the next option.
Vaginal tape surgery
The good news is SUI can be resolved with tension-free vaginal tape surgery – a simple procedure that causes minimal pain, has low complication rates and success rates of up to 95%.
It involves putting a permanent sling under the bladder neck. Both the patient and their spouse will not be able to feel the tape. This 10-minute surgery is done through the vagina and the patient can safely go home on the same day. More than 10,000 cases have since been performed with positive outcomes.
Pelvic organ prolapse
Just over 1 out of 10 women may suffer a pelvic organ prolapse in her lifetime. Pelvic organ prolapse can be mild, moderate or severe. When mild, the prolapse remains within the vagina. It is moderate if the prolapse is at the door of the vagina, and severe when the prolapse is outside the vagina. Once a prolapse has occurred, it will not recover on its own – it can only worsen. Pelvic floor exercises can help to prevent a prolapse from worsening but it will not cure it. Severe prolapse can be challenging to treat, and therefore it is important to diagnose the problem and seek treatment early.
Surgery for pelvic organ prolapse
Conventional surgery for severe bladder prolapse has a success rate of 70% at most, and most general gynaecologists do not perform these procedures.
Urogynaecologists use hitching surgical techniques and a net (mesh) to prevent recurrence. A success rate of 94.6% is possible when surgery is done with Prolene mesh, a polypropylene (plastic) mesh implant used to support and stabilise the vaginal wall and pelvic floor.
This technique requires special training, but when performed by an experienced surgeon, complications are minimal and success rates are high. As the surgery is done through the vagina, there are no scars, and the patient can be up and about in 1 – 2 days.
Infertility
The quality of eggs in females decreases gradually from the age of 25, more quickly after 35, and very steeply from 40.
Many couples face the problem of conception due to stress and starting a family at a later age. Fertility success rates decline with age, and pregnancy complications for the mum-to-be and the foetus increases. A third of fertility problems are due to female factors, a third to male factors and a third to both.
Couples are encouraged to consult a specialist for prenatal wellness checks if they experience unsuccessful conception after trying conscientiously for 6 – 12 months.
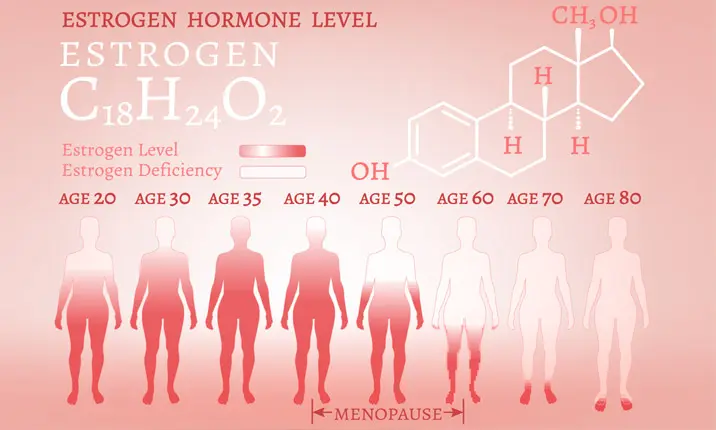
Menopause-related issues
Menopause is unavoidable, but the discomforts often associated with it can be alleviated. Symptoms include hot flushes, insomnia, mood swings, and depression. There are ways to effectively manage these symptoms and improve the woman's quality of life.
Osteoporosis
Menopause is also linked to increased risks of osteoporosis. The best way to combat this is through weight-bearing exercises. By adopting healthier lifestyle habits, such as not smoking and eating more calcium-rich foods (and even bone-forming medications, in certain cases), many fractures can be avoided.
Vaginal atrophy (dryness)
Another common issue experienced by menopausal women is vaginal atrophy (dryness), which can cause vaginal discomfort, frequent urination, and thinning of the vaginal and bladder tissues. This can lead to infection, and in many people, painful sex.
The latest treatment for vaginal atrophy is the FDA-approved laser vaginal treatment, a simple in-clinic procedure that causes minimal pain and complications, and has helped many patients, especially those facing problems with sexual intercourse.
Vaginoplasty
Although often a taboo topic, sexual intercourse is still regarded as an important part of a couple's relationship. Women with concerns about their sex lives are usually unaware that treatment can be simple and effective. Vaginoplasty, or the tightening of the vagina, in carefully selected cases, has helped many improve their sex lives. This surgery is done vaginally, as a day procedure with minimal pain and complications. It is important to seek treatment early so the couple can grow old, including sexually, together.
Prevention and early detection is key
Ladies, do not suffer in silence. Instead, empower yourselves. Do not be embarrassed to talk about your health issues. Many procedures are available to help you in simple, non-painful, non-complicated and yet very successful ways. Some are so simple but unfortunately, many do not know about these options or where to go for them.
It is important for women to go for yearly health checks. This will not only discover problems early, but can also help to prevent problems later. Sexually active women should go for regular cervical cancer screening. From the age of 40, women should consider going for a mammogram every 1 – 2 years to screen for breast cancer. After menopause, women (especially those in high-risk groups) can consider undergoing the bone density test to check for osteoporosis.
Prevention is better than cure. Have regular health checks and get treated early. It is possible to age gracefully, and live long – and well!