Total Hip Replacement (Total Hip Arthroplasty)
What is a total hip replacement?
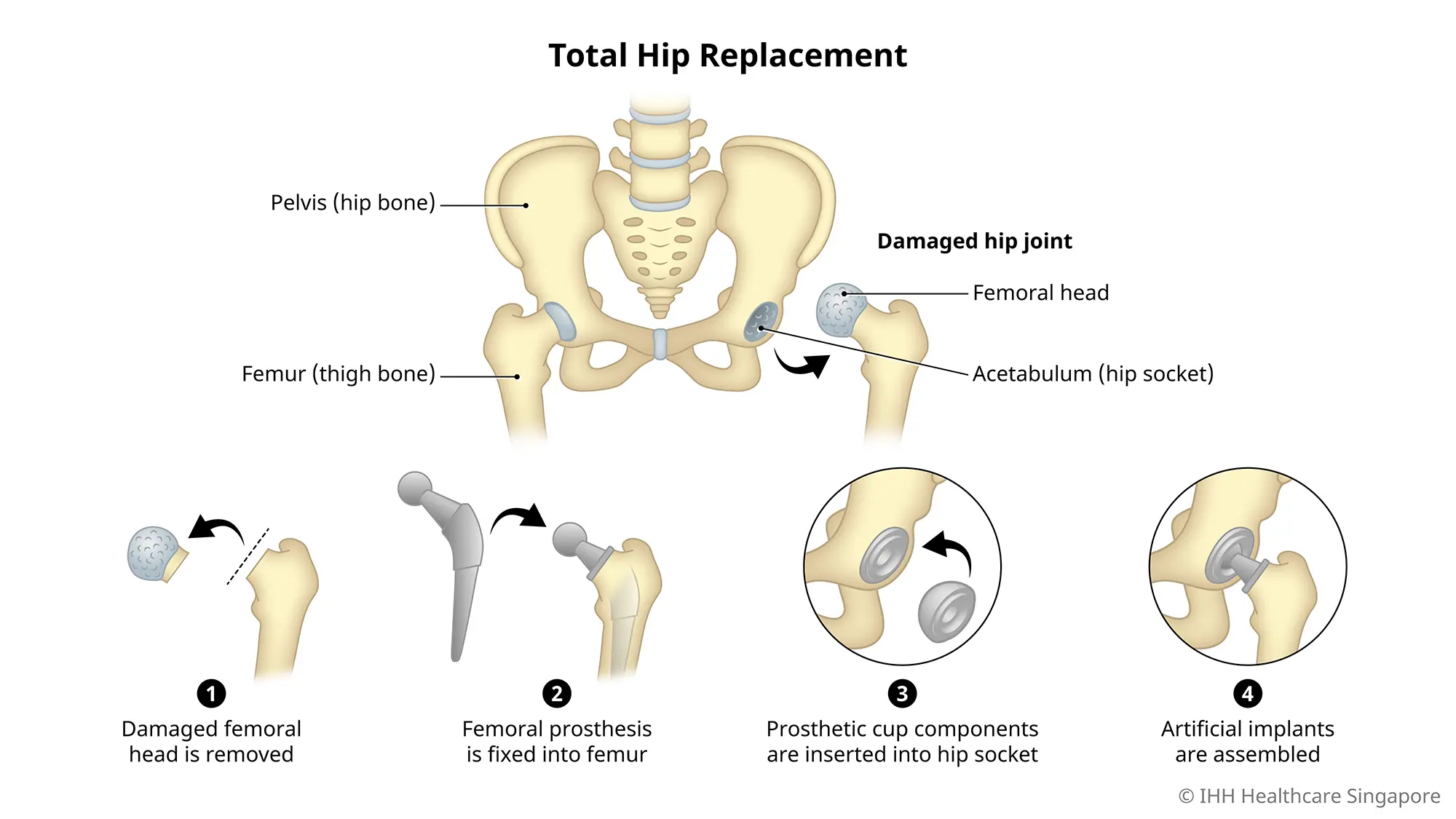
Total hip replacement, also known as total hip arthroplasty, is a surgical procedure that replaces the femur and the acetabulum with artificial joints.
During the procedure, your surgeon will replace the damaged or diseased 'ball and socket' joint with:
- An artificial femur (ball) made of strong metal or ceramic; and
- An artificial acetabulum (socket) made of a durable, wear-resistant plastic called polyethylene.
This artificial joint is designed to glide together to replicate the movement of the hip joint. With care, it can last around 20 years.
Ongoing improvements in surgical techniques and artificial joint materials may help these implants to last even longer.
Why do you need a total hip replacement?
You may consider hip replacement if:
- Conditions such as arthritis affect your everyday activities
- Non-surgical alternatives such as physiotherapy and anti-inflammatory medicines are unable to relieve hip pain
Conditions that may contribute to the need for hip replacement surgery include:
- Osteoarthritis, where a breakdown of cartilage (connective rubbery tissue) can lead to pain, swelling and deformity. Osteoarthritis occurs when damaged cartilage is unable to absorb shock or impact.
- Rheumatoid arthritis, a chronic inflammatory condition that leads to severe pain, stiffness and swelling that affects mobility.
- Osteonecrosis, where a lack of blood supply to the 'ball' portion of the hip joint may result in the collapse or deformity of the bone.
Hip replacement is only recommended after a careful diagnosis of your joint problem. With proper care after surgery, hip joint implants may last 20 years or longer.
What are the risks and complications of a total hip replacement?
Hip replacement surgery is a generally safe procedure. As with any form of surgery, a total hip replacement comes with some risks, such as:
- Blood clots in the leg veins due to limited walking during the initial period after surgery.
- Infection at the site of incision or in the deeper tissue near the new hip.
- Injury to nerves and blood vessels from swelling or pressure in and around the implant area.
- Need for additional surgeries due to the loosening of the new joint over time.
- Dislocation of the ball of the new joint from its socket due to moving or resting in the wrong position.
Those with severe rheumatoid arthritis, systemic lupus, diabetes or haemophilia may face a higher risk of complications. You are encouraged to speak with your surgeon to understand if this surgery is right for you.