How do falls affect the elderly?
Orthogeriatrics, or geriatric orthopaedics, refers to the management of orthopaedic problems (disorders in the bones, joints, muscles, tendons and ligaments) in the elderly. Your risk of orthopaedic issues such as hip fractures, osteoporosis and osteoarthritis increases with age, and these medical conditions are a leading cause of falls among the elderly.
In orthopaedic care for the elderly, osteoporosis and osteoarthritis are 2 of the main issues.
What is osteoporosis?
Osteoporosis is a bone condition which occurs when bones lose their strength and mass. This happens when bone tissue is lost at a higher rate than it is produced. As this happens, bones become more fragile and prone to fracture. Bones in the hip, spine and wrist are particularly susceptible to fractures.
Symptoms of osteoporosis
Described as a "silent disease", there are generally no symptoms in the early stages of this condition. At an advanced stage, you may experience symptoms such as:
- Back pain (especially in the lower back)
- A stooped posture, with height loss over time
- Increased proneness to fractures in the hip, spine and wrist
Causes of osteoporosis
Factors that increase your risk of developing osteoporosis include:
- Menopause – twice as many women than men have osteoporosis. Women are more prone to developing osteoporosis as up to 20% of bone mass can be lost in the 5 – 7 years after menopause. Women with early menopause before 45 years old are also at risk
- Being Caucasian or Asian – studies show that around 20% of Asian and Caucasian women above 50 years old have osteoporosis, while 52% have decreased bone mass, which is a precursor to osteoporosis
- Being older – generally, our bone mass peaks in our 20s, and begins to decrease after
- Having a family history of osteoporosis
- Insufficient intake of vitamin D and calcium
- Being underweight weakens bones in both men and women and is therefore likely to lead to osteoporosis
- Having certain illnesses, such as rheumatoid arthritis and thyroid problems
- Taking certain medication, such as thyroid medication and corticosteroids (usually prescribed to treat diseases such as asthma and arthritis)
Treating osteoporosis
Osteoporosis is highly treatable. To treat osteoporosis, your doctor may prescribe medication such as bisphosphonates, calcium, and vitamin D supplements to help increase bone density.
Preventing osteoporosis
To prevent osteoporosis, it is important to exercise regularly to build stronger and denser bones, and observe a healthy diet. Avoid excessive consumption of alcohol, caffeine and sodium as these foods can lead to bone loss and/or affect bone formation.
What is osteoarthritis?
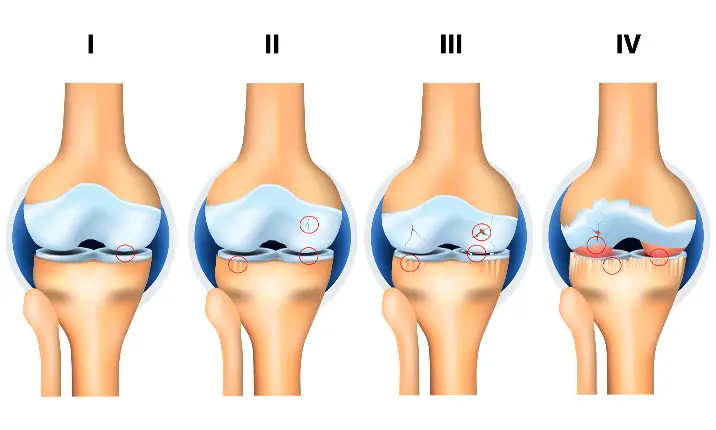
Osteoarthritis is a degenerative condition of the joints, and is the most common form of arthritis (inflammation of the joints). It occurs when the protective cartilage at the end of bones is worn down, causing the bones in our joints to rub against one another. Although those above 60 are more likely to be affected by osteoarthritis, an increasing number of younger and active Singaporeans have been diagnosed with premature osteoarthritis from sports injuries.
Symptoms of osteoarthritis
Osteoarthritis usually develops slowly and increases in severity over time. While osteoarthritis can occur in any joint, it commonly affects joints in the hands, knees, hips and spine. Common symptoms include pain, stiffness, tenderness, loss of flexibility, swelling and a grating sensation in our joints.
Causes of osteoarthritis
Factors that increase your risk of developing osteoarthritis include:
- Age – as we age, our joint cartilage is more likely to experience wear-and-tear, resulting in osteoarthritis
- Gender – females have a higher risk of developing osteoarthritis than men. While the reason behind this is unclear, it may be related to hormonal differences between men and women
- Trauma from sports injuries such as anterior cruciate ligament (ACL) strains and tears, torn cartilages, dislocated joints and ligament injuries can cause osteoarthritis, even if you have since healed from these injuries
- Being overweight puts an individual at higher risk especially for developing knee osteoarthritis, which can be potentially treated with weight loss
- Hereditary – having a family history of osteoarthritis
Treating osteoarthritis
To treat osteoarthritis, doctors can undertake cartilage repair procedures and complete joint replacement procedures in severe cases.
Preventing osteoarthritis
Losing weight, doing low-impact exercises and taking joint supplements such as glucosamine regularly can help to slow down the development of osteoarthritis.
Elderly falls: Osteoporosis and osteoarthritis risk factors
Osteoporosis and osteoarthritis are two conditions that can lead to mobility issues among the elderly, increasing their chances of falling.
Falls are common among older adults and can cause minor injuries such as bruises and scratches. However, more severe falls may result in serious injuries such as fractures and head trauma. These can lead to reduced physical function, early admission to long-term care facilities, and an increase in elderly mortality rates.
Osteoporosis risk factors
- Osteoporosis can lead to poor balance causing a person difficulty when trying to steady themselves after tripping, resulting in a fall
- Osteoporosis means a decrease in bone density, which makes bones brittle and more prone to breakage
Osteoarthritis risk factors
- Osteoarthritis causes pain which may cause a person to avoid the use of certain joints. This may result in unsteadiness and weakness leading to falls
- Osteoarthritis can cause joint rigidity, which may affect how you walk or move
- Certain pain medications taken for osteoarthritis, such as opioids may cause side effects like dizziness and drowsiness that can contribute to falls
Preventing elderly falls
While younger people can make speedy recoveries from falls, the recovery time for an elderly takes much longer, depending on the severity of the fall and their health condition. Therefore, it is important to senior-proof your surroundings, as well as ensuring that older people have the necessary assistance when moving about.
Some tips to prevent elderly falls include:
1. Remove hazards around the home.
The simplest way to reduce your likelihood of falls is to remove loose items such as electrical wires, slippery rugs, and clutter. Hazardous house fixtures such as uneven floorboards are some examples of things that can cause tripping.
2. Install safety devices in your home.
Installing safety devices such as handrails and grab bars in areas such as toilets and stairways can go a long way in supporting your mobility around the home. Non-slip mats are a good option to prevent slipping in the bathroom.
3. Ensure your house is adequately lit.
Keeping your home sufficiently bright can reduce your chances of tripping over objects on the ground. Consider putting lights (such as lamps, ceiling lights or torch lights) around areas like your bedrooms, bathrooms and stairways.
4. Consult your doctor.
Your doctor can work with you to craft a fall-prevention plan. Your doctor can review aspects of your lifestyle and health such as your medication and existing medical conditions (e.g. eye and ear disorders) that may be contributing to your risk of falling.
5. Have company around.
Ensure that someone is accompanying or assisting you especially when you are going out or walking longer distance
6. Get a walking aid.
Use a walking aid or walker and keep an emergency tag, phone, or keyring with you.
7. Review medications.
Go through your medications with your doctor and review their side effects so that you can look for alternatives if the drugs make feel you drowsy.
Final Advice
Both osteoporosis and osteoarthritis are treatable conditions which left untreated, can increase your risk of falling. Do consult a doctor early if you suspect that you may have either condition.