What is cardioversion?
Cardioversion is a procedure in which an abnormally fast heart rate is converted to a normal rhythm using electricity or drugs.
Types of cardioversion include:
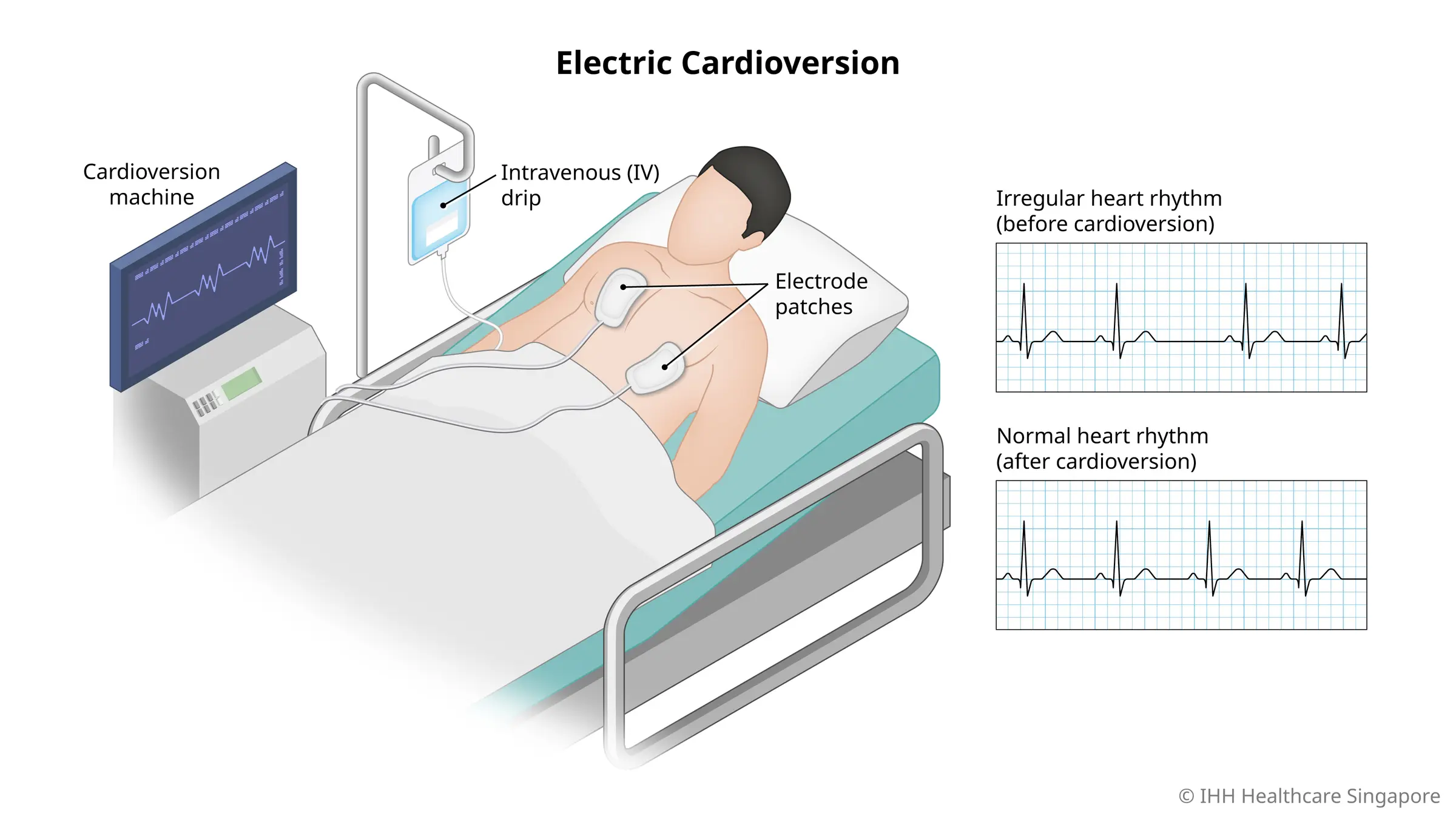
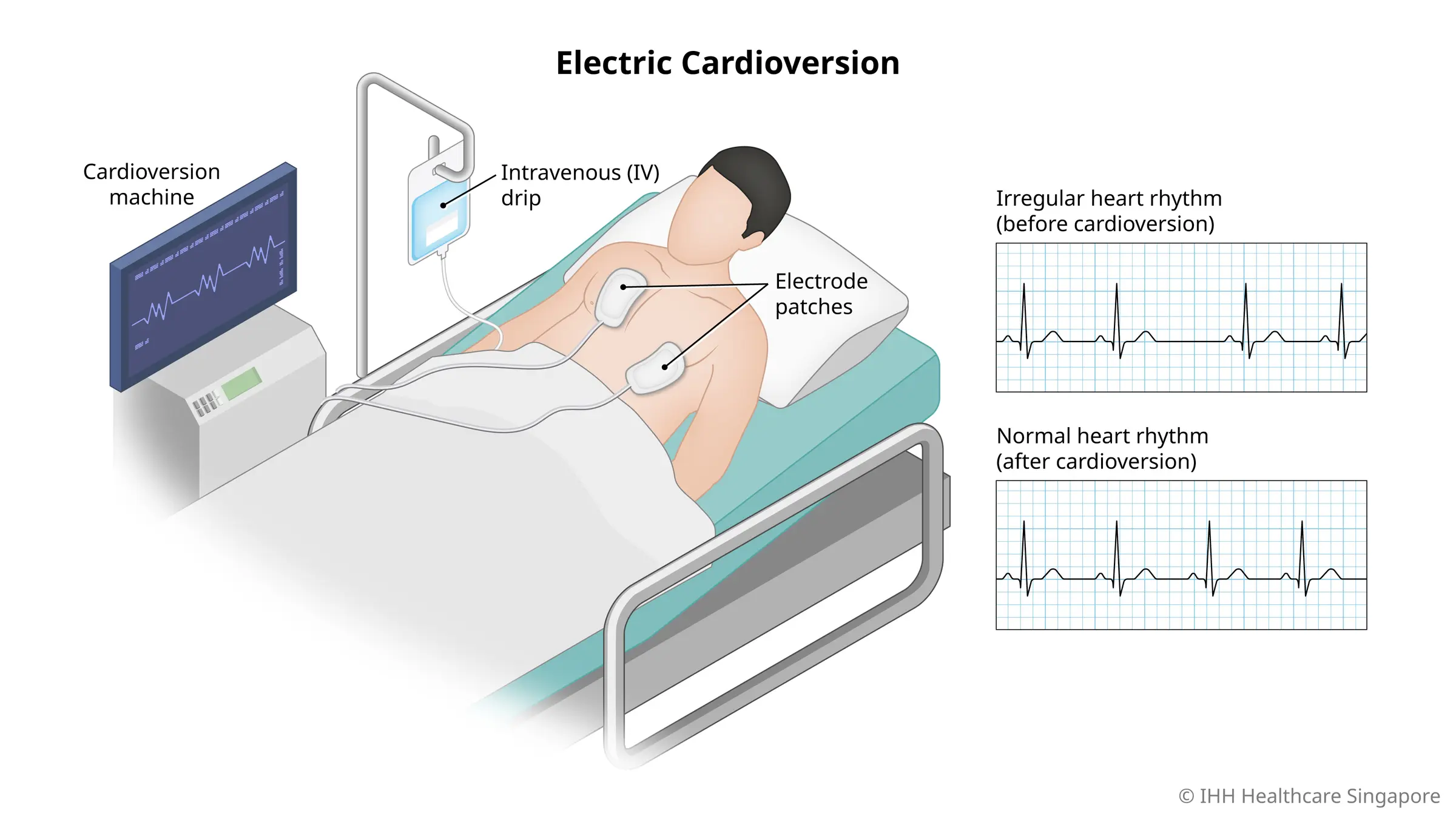
- Electric cardioversion - Where a high-energy shock is sent to the heart to reset a normal rhythm, through paddles or electrodes attached to the chest while you are under sedation
- Pharmacologic or chemical cardioversion - Uses medication instead of an electrical shock to restore your heart’s rhythm
Electric cardioversion takes less time than pharmacologic or chemical cardioversion.
Cardioversion can quickly restore a regular heartbeat for most people. However, you will likely need additional procedures or medication after the cardioversion to maintain a normal heart rhythm.
Why do you need a cardioversion?
Cardioversion is used to correct a heartbeat that is too fast (tachycardia) or more commonly, irregular heart rhythms (atrial fibrillation or AFib).
The goal of irregular heart rhythm treatment is to restore normal heart rhythm where possible and reduce the risk for serious complications and heart disease.
Your doctor will consider factors such as your age and overall heart health to determine whether cardioversion is an appropriate treatment for you.
What are the risks and complications of cardioversion?
While complications of cardioversion are not common, it does have certain risks, such as:
- Abnormal heart rhythm, a rare occurrence where you develop other abnormal heart rhythms during or after the procedure
- Dislodged blood clots, which can cause stroke, pulmonary embolism (blood clot travelling to your lungs), or other problems
- Skin damage, where you have minor burns on the areas of your skin where the electrodes were placed
- Reaction to general anaesthesia or sedation, if used
Your doctor may give you blood thinners to help prevent clots, and take other necessary steps to lower your risks.
Note: While cardioversion can be done during pregnancy, your doctor will need to monitor the baby's heartbeat during the procedure.
How do you prepare for a cardioversion?
To prepare for the procedure, your doctor will:
- Order several tests to evaluate your heart condition
- Discuss with you the risks and benefits of your treatment
- Need to know about your allergies or reactions to medications
Before the procedure, you will need to:
- Go on an overnight fast, or fast for at least 6 hours before the cardioversion
- Inform your doctor about all the medications you are taking, including prescriptions, vitamins, minerals, herbs, drugs or any other supplements
- Inform your doctor if you have an implanted heart device, such as a pacemaker or implantable cardioverter-defibrillator, so that your doctor can take any additional precautions if needed
What can you expect for a cardioversion?
Electric cardioversion is done on an outpatient basis. You will be able to go home on the same day of your procedure.
Estimated duration
The procedure lasts only a few minutes, although additional time will be required for the set up and sedation or general anaesthesia.
During the procedure
The procedure can be broken down into the following steps:
- You will receive medications through an IV to make you fall asleep so that you will not feel any sensations from the shocks during the procedure.
- You may also be given other medications through the IV to help restore your heart rhythm.
- Several large patches called electrodes connect to a cardioversion machine (defibrillator) will be placed on your chest.
- The cardioversion machine will send a programmed high-energy shock to your heart to convert your heart back to a normal rhythm.
- Your heart rhythm will be closely monitored. You will also be watched for any signs of complications.
- A transesophageal echocardiogram may be arranged just before the cardioversion to confirm that there are no blood clots in your heart that can increase the risk of stroke.
After the procedure
In case there are complications, you will need to spend about an hour in a recovery room under observation.
Do arrange for someone to drive you home after the recovery period.
After you have left the hospital, you may want to take note of the following:
- Your ability to make decisions may be affected for several hours after your procedure.
- You may need to take blood-thinning medications for at least several weeks after your procedure even if no clots were found in your heart before your procedure. This is to prevent new clots from forming.
You may experience some side effects of the treatment, such as:
- Diarrhoea
- Nausea
- Vomiting
- Hypotension
- Heart failure
- Tremor
- Headache
- Depression
- Seizures
Care and recovery for a cardioversion
Your irregular heart rhythm may recur after your treatment, especially if you are:
- Older
- Have other heart conditions
- Have high blood pressure
- Have a history of difficult-to-treat atrial fibrillation
After the procedure, you will likely have a follow-up appointment with your doctor about 1 week to 3 months later, depending on the clinical situation and arrhythmia.
If your atrial fibrillation returns, your doctor may:
- Need to control it with medications
- Recommend that you undergo another procedure, such as catheter ablation
- Recommend a permanent pacemaker
Your doctor may also recommend that you participate in cardiac rehabilitation to help you improve your health and recover after heart surgery.