Health Plus articles
Is Your Breast Lump Cancerous? Identifying Types and Symptoms
Worried about that strange lump on your breast? We delve into its most common causes.
What Are Minor Surgeries And When Are They Required?
Find out more about minor surgeries and when they may be necessary.
How to Eat Well for Post-Surgery Recovery
Nutrition plays an important role in your recovery after surgery. Knowing what foods to eat after going for an operation may help to improve and speed up your healing process.
Metabolic Surgery for Diabetes: Frequently Asked Questions
Metabolic surgery is shown to cure metabolic diseases such as type 2 diabetes.
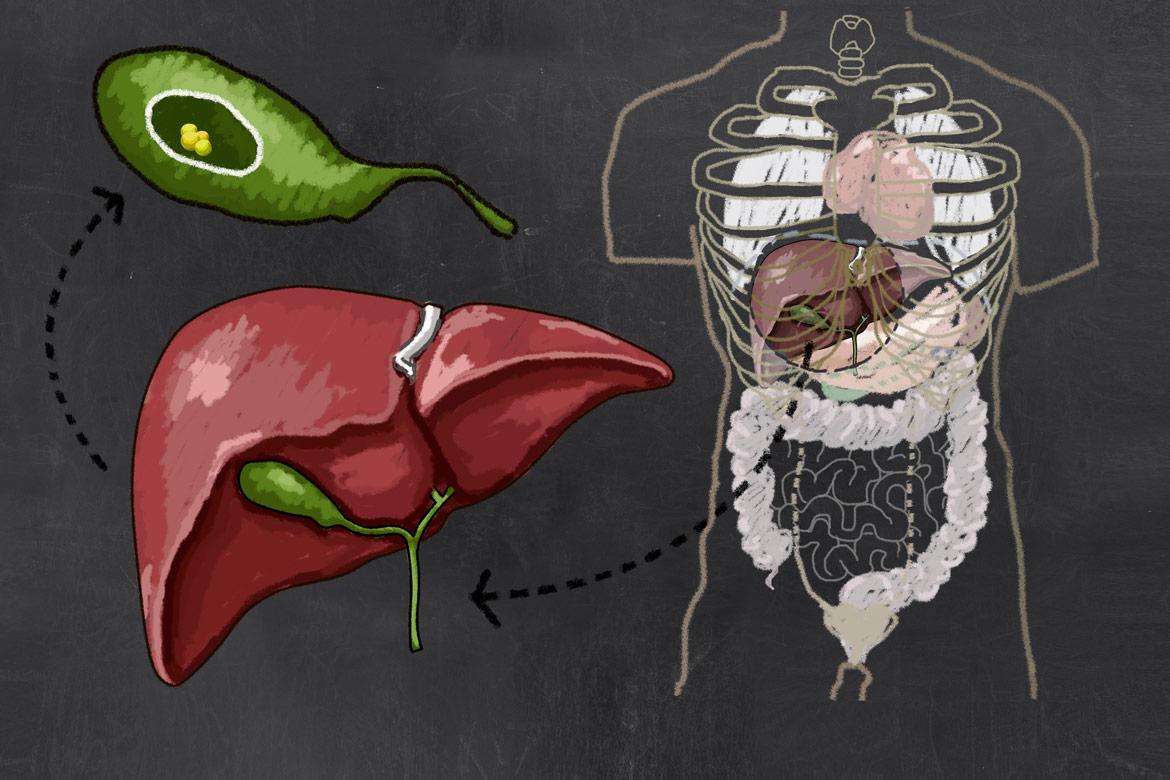
Gall Bladder Removal Surgery for Gallstones
Find out when gall bladder removal surgery is recommended for those suffering with gallstones.
Can a Gastroscopy or Colonoscopy Help Prevent Cancer?
We discuss the role gastroscopies and colonoscopies play in cancer prevention and what they entail.